Gianluca
Well-Known Member
Really?
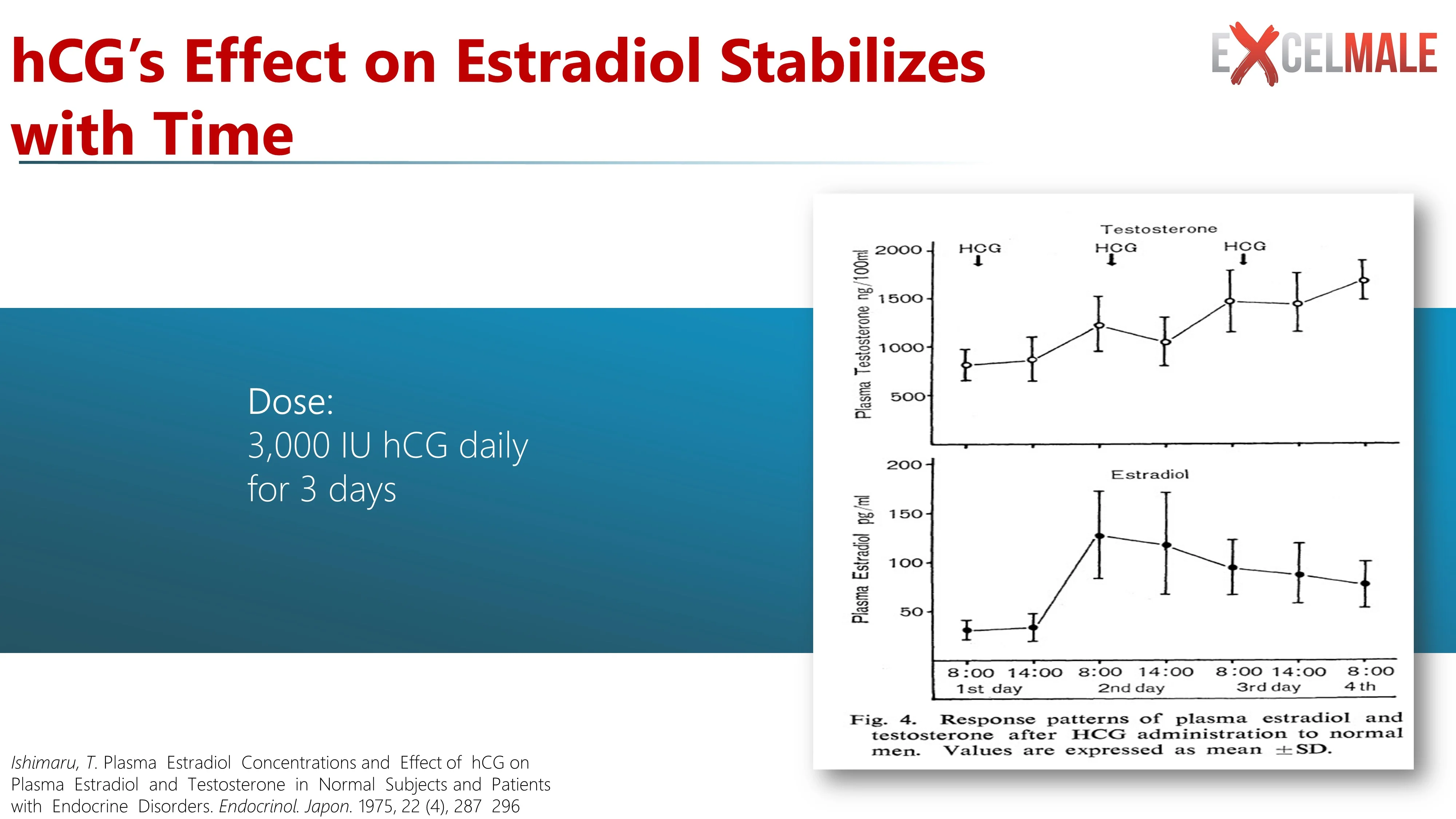
hCG mimics LH which stimulates Leydig cells leading to an increase in both ITT (intratesticular testosterone) and circulating testosterone levels.
LH is critical as it stimulates cAMP production and cholesterol transport to and metabolism within mitochondria.
post#37

Playing with HCG gave me libido - Page 2 - Excel Male TRT Forum
Current protocol: 75mg sustanon once weekly. 75 FSH EOD 500 HCG EOD last three weeks I had a great improvement in libido. i switched to 250 HCG and got one week of amazing libido. Week after that I went back to 500 nothing happened. This week I went again to 250 and stretched it to E3D and...www.excelmale.com
My reply:
The main purpose of adding hCG to trt is to preserve/maintain fertility and prevent/minimize testicular atrophy.
The use of exogenous testosterone results in the suppression of ITT (intra-testicular testosterone) which is critical for sperm production.
The main goal when using hCG is to restore physiological ITT levels and in order to achieve such a minimum effective dose would be needed (125-500IU) and 250-500IU would seem to be the sweet spot.
Anything less will have a minimal impact on increasing ITT!
Other than one experiencing possible side effects from such doses (250-500IU) using anything <125IU will have a minimal impact on increasing ITT.
My reply from a previous thread where the poster asked if hCG was needed.
Depends on the individual.....Is hCG needed?
*To preserve/maintain fertility then yes.
*To prevent/minimize testicular atrophy then yes.
*To enhance mood/libido than it is not a given as some may experience such effects whereas others may feel worse-off.
*To maintain upstream hormones and possibly prevent long-term consequences for health/well-being.....you be the judge!
Effect of TRT vs hCG/FSH on upstream hormone pathways.
The role of gonadotropins in testicular and adrenal androgen biosynthesis pathways -insights from males with congenital hypogonadotropic hypogonadism on hCG/rFSH and on testosterone replacement SUMMARY Objective: To delineate the role of gonadotropins in male androgen biosynthesis pathways...www.excelmale.com
*take-home point
A replacement regimen with combined hCG/rFSH mimics physiologic steroid hormone profiles better than a substitution with exogenous testosterone. The documented differences in steroid profiles on testosterone replacement in hypogonadal males with absent or severely reduced endogenous LH and FSH secretion may have long-term consequences for health and wellbeing. Specifically, body composition, bone health, glucose, and lipid metabolism, salt and water balance, cognition, mood, sleep, and sexual function could be affected. The steroidogenic differences could also be relevant for gonadotropin-suppressive treatments with long-acting testosterone preparations in males with primary hypogonadism. To what extent this hypothesis is true, should be addressed in future clinical studies.
Testosterone synthesis in Leydig cells
Steroidogenesis is a multi-step process that converts cholesterol into final steroid hormone products. As reviewed in Aghazadeh and coworkers (Aghazadeh et al. 2015), steroidogenesis consists of cholesterol mobilization from lipid droplets and/or the plasma membrane, cholesterol transport into mitochondria, pregnenolone formation in the mitochondria, and subsequent conversion of pregnenolone into the final steroid products by enzymes of the smooth endoplasmic reticulum (Fig. 1). In the adult testis, Leydig cell TS production depends upon the pulsatile secretion of LH by the pituitary gland into the peripheral circulation. LH plays two essential roles in Leydig cell steroidogenesis: (1) maintenance of optimal levels of steroidogenic enzymes (trophic regulation) and (2) mobilization and transport of cholesterol into the inner mitochondrial membrane (acute regulation).
View attachment 15215
Leydig cell steroidogenesis.
LH binds its receptor on the Leydig cell membrane. LH receptor/G protein coupling results in increased cAMP and arachidonic acid (AA) production. cAMP stimulates the mobilization and transport of cholesterol to and into the mitochondria in part by activating PKA and MAPK signaling. At the same time, AA can be converted into prostaglandin by Cox2 to negatively regulate the transport of cholesterol across the mitochondrial membranes. At the inner mitochondrial membrane, cholesterol is converted to pregnenolone by CYP11A1, and pregnenolone is converted into testosterone by enzymes in the smooth endoplasmic reticulum (HSD3b, CYP17A1, and HSD17b). Aging and environmental factors may impact steroidogenesis by affecting the intracellular redox balance in part through increased ROS production. This has significant effects on the cAMP formation and/or cholesterol transport into the mitochondria, and thus on steroid formation. Steroidogenesis also might be affected by ROS-induced increases in Cox2 production and redox-sensitive MAPK activation.
Both the trophic and acute effects of LH are mediated by signaling pathways that begin with cAMP production (Fig. 1). LH binds to and activates G protein-coupled receptors, resulting in the activation of adenylyl cyclase, increased intracellular cAMP formation, and cAMP-dependent phosphorylation of proteins through protein kinase A (PKA). The acute stimulation of Leydig cells by LH results in cholesterol transfer into the mitochondria in part through the actions of steroidogenic acute regulatory protein (STAR), translocator protein (18 kDa; TSPO), and other proteins of the transduce some (Midzak et al. 2011). Cholesterol transport into the mitochondria, the rate-limiting step in steroid biosynthesis, is followed by the conversion of cholesterol to pregnenolone by the C27 cholesterol side-chain cleavage cytochrome P450 enzyme (CYP11A1) located on the matrix side of the inner mitochondrial membrane. Pregnenolone then is metabolized into TS by 3β-hydroxysteroid dehydrogenase (3b-HSD; HSD3B), 17α-hydroxylase/17,20 lyase (CYP17A1) and type 3 17β-hydroxysteroid dehydrogenase (17b-HSD3, HSD17B) in the smooth endoplasmic reticulum (Payne & Hales 2004, Aghazadeh et al. 2015, Beattie et al. 2015).
YES THERE IS NO NEED FOR HCG TO INCREASE PREGNENOLONE LEVEL, as you can see even form the recent Nelson report, Pregnenolone supplementation does a better job.