I started trt due to having low testosterone 3 years ago. From the first day of starting trt I have never felt good. Always felt snappy and moody. I have tried testosterone E. P. C. Nebido and cream. It seems I do not aromatize from the testosterone and I am a hyper responder to the testosterone. My libido has been zero since starting the testosterone treatment which is probably due to the low E2. I have recently read that dianabol can be taken instead of testosterone. Also a benefit of dianabol is raised E 2 which possibly could help my libido.... Does anybody have any other positive information on dianabol if taken in small doses.. thanks
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Deleted member 43589
Well-Known Member
CIBA withdrew Dianabol from the U.S. market in 1983. Generic production shut down two years later, when the FDA revoked metandienone's approval entirely in 1985. Now me being a realist, I know it is not that hard to find metandienone in a variety of doses. That being said:
K. Remes,P. Vuopio,M. Järvinen,M. Härkönen &H. Adlercreutz. Effect of short-term treatment with an anabolic steroid (methandienone) and dehydroepiandrosterone sulphate on plasma hormones, red cell volume and 2,3-diphosphoglycerate in athletes. Scandinavian Journal of Clinical and Laboratory Investigation 39:8 Pages 577-586 | Received 04 Feb 1977, Accepted 27 Jun 1977, Published online: 08 Jul 2009. https://doi.org/10.3109/00365517709100649
Abstract
The effects of a one-month course of treatment with a potent anabolic steroid, methandienone (5 and 10 mg daily), and a very weak androgen and hormone precursor, dehydroepiandrosterone sulphate (DHEAS, 20 and 40 mg daily) and placebo on plasma testosterone, LH and FSH levels, red cell volume and red cell 2,3-diphosphoglycerate (2,3-DPG) concentration in endurance sportsmen were studied using a double-blind test system. A highly significant decrease in mean plasma testosterone was observed after the 5 and 10 mg methandienone regimen (66 and 73%). Treatment with 40 mg of DHEAS decreased mean testosterone levels by 41% (not statistically significant). Pre-test testosterone levels were reattained about 10 days after the end of the treatment period with the higher doses of both compounds, while 2–6 weeks afterwards a significant over-compensation in mean plasma testosterone levels was observed. No significant changes in plasma gonadotropins were seen immediately after treatment with either of these steroids but later a tendency towards decreased FSH and LH levels was observed in the subjects who received the higher doses of both compounds. No significant changes in red cell volume were observed. Red cell 2,3-DPG concentration was unaffected by methandienone, but the 40 mg dosage of DHEAS caused a highly significant decrease in 2,3-DPG (by 26%, which is an unwanted effect for top sportsmen).
K. Remes,P. Vuopio,M. Järvinen,M. Härkönen &H. Adlercreutz. Effect of short-term treatment with an anabolic steroid (methandienone) and dehydroepiandrosterone sulphate on plasma hormones, red cell volume and 2,3-diphosphoglycerate in athletes. Scandinavian Journal of Clinical and Laboratory Investigation 39:8 Pages 577-586 | Received 04 Feb 1977, Accepted 27 Jun 1977, Published online: 08 Jul 2009. https://doi.org/10.3109/00365517709100649
Abstract
The effects of a one-month course of treatment with a potent anabolic steroid, methandienone (5 and 10 mg daily), and a very weak androgen and hormone precursor, dehydroepiandrosterone sulphate (DHEAS, 20 and 40 mg daily) and placebo on plasma testosterone, LH and FSH levels, red cell volume and red cell 2,3-diphosphoglycerate (2,3-DPG) concentration in endurance sportsmen were studied using a double-blind test system. A highly significant decrease in mean plasma testosterone was observed after the 5 and 10 mg methandienone regimen (66 and 73%). Treatment with 40 mg of DHEAS decreased mean testosterone levels by 41% (not statistically significant). Pre-test testosterone levels were reattained about 10 days after the end of the treatment period with the higher doses of both compounds, while 2–6 weeks afterwards a significant over-compensation in mean plasma testosterone levels was observed. No significant changes in plasma gonadotropins were seen immediately after treatment with either of these steroids but later a tendency towards decreased FSH and LH levels was observed in the subjects who received the higher doses of both compounds. No significant changes in red cell volume were observed. Red cell 2,3-DPG concentration was unaffected by methandienone, but the 40 mg dosage of DHEAS caused a highly significant decrease in 2,3-DPG (by 26%, which is an unwanted effect for top sportsmen).
1. Do blood tests, no assumptions about "probably low E2"
2. Dbol is indeed excellent for raising E2, specifically methyl E2 which is even more potent than E2.
3. Dbol cannot be taken in isolation as it is not test, does not contain test and does not replace test.
4. Dbol cannot be used longer than a few weeks due to hepatotoxicity. For example bodybuilders therefore use dbol for around 4 weeks at a time, after which point it is shown that liver enzymes are elevated. Continued use leads to dark orange and then brown piss and jaundice. Not good things.
5. If low E2 is indeed an issue, small amounts of dbol along with TRT can be used short term just to test how you feel on it, so that you may glean clues as to how you feel on what.
6. Trestolone/MENT has very similar subjective effects to dbol, but is injectable and lacks the liver side effects, allowing continued use.
2. Dbol is indeed excellent for raising E2, specifically methyl E2 which is even more potent than E2.
3. Dbol cannot be taken in isolation as it is not test, does not contain test and does not replace test.
4. Dbol cannot be used longer than a few weeks due to hepatotoxicity. For example bodybuilders therefore use dbol for around 4 weeks at a time, after which point it is shown that liver enzymes are elevated. Continued use leads to dark orange and then brown piss and jaundice. Not good things.
5. If low E2 is indeed an issue, small amounts of dbol along with TRT can be used short term just to test how you feel on it, so that you may glean clues as to how you feel on what.
6. Trestolone/MENT has very similar subjective effects to dbol, but is injectable and lacks the liver side effects, allowing continued use.
Guided_by_Voices
Well-Known Member
Dbol also has a very short half life (5 hours I think) so it is unlikely to be a long term solution although if it helped briefly, it could be a clue that estrogen is indeed your issue. More importantly, you didn't give an info on your protocol or bloodwork, which are likely much better indicators. Many people do better on lower TRT doses so that is one place to investigate. Some people do better with higher DHT levels (not me) so that is something else to investigate.
Thanks for that much appreciated. I'm a hyper responder to test but it's a bit raising my E2 . . I only take 100 mg a week if test E . Was hoping the dianabol might boost E2 to help libdio which is dead. Prolactin and thyroid are fine ... Would trestolone boost my E2 ?. having a poss boost in my libido ,?1. Do blood tests, no assumptions about "probably low E2"
2. Dbol is indeed excellent for raising E2, specifically methyl E2 which is even more potent than E2.
3. Dbol cannot be taken in isolation as it is not test, does not contain test and does not replace test.
4. Dbol cannot be used longer than a few weeks due to hepatotoxicity. For example bodybuilders therefore use dbol for around 4 weeks at a time, after which point it is shown that liver enzymes are elevated. Continued use leads to dark orange and then brown piss and jaundice. Not good things.
5. If low E2 is indeed an issue, small amounts of dbol along with TRT can be used short term just to test how you feel on it, so that you may glean clues as to how you feel on what.
6. Trestolone/MENT has very similar subjective effects to dbol, but is injectable and lacks the liver side effects, allowing continued use.
Last bloods done in march. . so new ones are due next week...You still haven't posted blood results confirming that your E2 is indeed low.
Nonetheless, yes, trestolone aromatises to potent methyl E2 .
Will this solve your libido? Thats anyones guess
Attachments
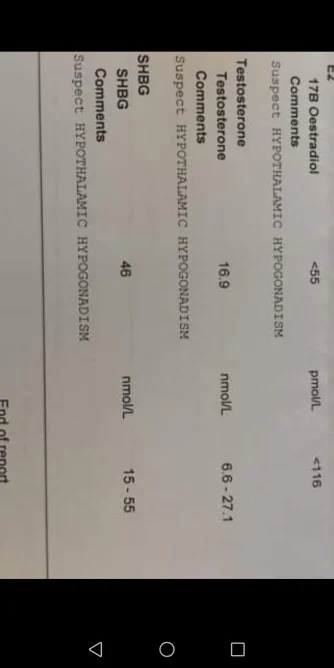
I do 100 mg split twice a week. Here are my last bloods from march this year .... I I'm currently having high BP .. 135/ 85.. three years and still I've not had any benefit from testDbol also has a very short half life (5 hours I think) so it is unlikely to be a long term solution although if it helped briefly, it could be a clue that estrogen is indeed your issue. More importantly, you didn't give an info on your protocol or bloodwork, which are likely much better indicators. Many people do better on lower TRT doses so that is one place to investigate. Some people do better with higher DHT levels (not me) so that is something else to investigate.
I take 100 mg a week split between two days . I'm currently having high BP issues. Fuzzy head with 135/85 . Thinking I've had no benefits from being on trt three years . May be it's time to stop it all ...Dbol also has a very short half life (5 hours I think) so it is unlikely to be a long term solution although if it helped briefly, it could be a clue that estrogen is indeed your issue. More importantly, you didn't give an info on your protocol or bloodwork, which are likely much better indicators. Many people do better on lower TRT doses so that is one place to investigate. Some people do better with higher DHT levels (not me) so that is something else to investigate.
Attachments
Deleted member 43589
Well-Known Member
Back when I did anabolic steroids for muscle gain.....anytime we did a highly anabolic drug, we also did testosterone with it as a base. While the anabolic lowered blood testosterone levels, the added androgenic effect of testosterone solved the problem.Thanks for that much appreciated. I'm a hyper responder to test but it's a bit raising my E2 . . I only take 100 mg a week if test E . Was hoping the dianabol might boost E2 to help libdio which is dead. Prolactin and thyroid are fine ... Would trestolone boost my E2 ?. having a poss boost in my libido ,?
Trestolone is thought to be capable of sustaining normal male physiology in the complete absence of testosterone, including sexual functioning. Despite being in the 19-nor family of steroids. But like trestolone, it has the ability to aromatize, much more than testostereone. Most guys I have known who used it blew up very quickly.
Thank you very very much for that information. I really appreciate your words.. it's definitely something to look at as the testosterone I'm taking now and have been for 3 years has never made me feel good and has never helped my libido. Thank youBack when I did anabolic steroids for muscle gain.....anytime we did a highly anabolic drug, we also did testosterone with it as a base. While the anabolic lowered blood testosterone levels, the added androgenic effect of testosterone solved the problem.
Trestolone is thought to be capable of sustaining normal male physiology in the complete absence of testosterone, including sexual functioning. Despite being in the 19-nor family of steroids. But like trestolone, it has the ability to aromatize, much more than testostereone. Most guys I have known who used it blew up very quickly.
madman
Super Moderator
I started trt due to having low testosterone 3 years ago. From the first day of starting trt I have never felt good. Always felt snappy and moody. I have tried testosterone E. P. C. Nebido and cream. It seems I do not aromatize from the testosterone and I am a hyper responder to the testosterone. My libido has been zero since starting the testosterone treatment which is probably due to the low E2. I have recently read that dianabol can be taken instead of testosterone. Also a benefit of dianabol is raised E 2 which possibly could help my libido.... Does anybody have any other positive information on dianabol if taken in small doses.. thanks
You need to post your most recent labs.
Weare flying blind here.
Need to know where your trough TT, FT, and estradiol sit let alone RBCs/hemoglobin/hematocrit.
Hopefully, you tested using the most accurate assays TT/estradiol (LC/MS-MS) and FT (Equilibrium Dialysis or Ultrafiltration).
You have highish SHBG so it is critical that you tested using an accurate assay.
Methandrostenolone could never replace testosterone let alone it is not something that one would use long-term due to the compound being c-17 alpha alkylated which is known to stress the liver.
The use of AAS 17α-alkylated orals such as stanozolol, oxandrolone, methyltestosterone, methandrostenolone, oxymetholone, and fluoxymesterone are notorious for driving down HDL, increasing LDL, stressing the liver and hammering down SHBG.
Even then the dose/duration of use will play a big role.
Highly doubtful you are going to run into any serious liver damage from using therapeutic does (oxandrolone/stanazolol) let alone low doses of any other c-17 alpha alkylated orals from short-term use.
No AAS would be a substitution for testosterone.
If anything there may be some merit in using 7α-methyl-19-nortestosterone (MENT) which appears to be an appropriate candidate for androgen substitution in hypogonadal men as it possesses high androgenic potency and aromatizes to 7amethylestradiol.
Mind you it is not converted to DHT let alone the studies done were on a small number of patients who were using extremely low doses (subcutaneous implants/transdermal gel) and they were not long-term (>1 yr).
Hard to say what impact this would have as a sole replacement long-term especially when it comes to libido/brain chemistry.
If you feel comfortable giving it a shot go nuts!
The main reason testosterone is used for replacement therapy over nandrolone let alone any other AAS is that testosterone drugs provide a hormone that is already produced in the body.
Let alone metabolites estradiol and DHT are needed in healthy amounts to experience the full spectrum of testosterones beneficial effects on (cardiovascular health, brain health, libido, erectile function, bone health, tendon health, immune system, lipids, and body composition).
*Natural testosterone is viewed as the best androgen for substitution in hypogonadal men. The reason behind the selection is that testosterone can be converted to DHT and E2, thus developing the full spectrum of testosterone activities in long-term substitution
*Preparations of native testosterone or its esters (aromatizable T) should be used for TTh
The history of discovery, synthesis, and development of testosterone for clinical use (2015)
Eberhard Nieschlag and Susan Nieschlag
Abstract
As the most important male hormone, testosterone has an impact on almost all organs and body functions. The biological effects of testosterone and the testes have been known since antiquity, long before testosterone was identified as an active agent. Practical applications of this knowledge were the castration of males to produce obedient servants, for punishment, for the preservation of the prepubertal soprano voice, and even for the treatment of diseases. Testes were used in organotherapy and transplanted as a treatment for symptoms of hypogonadism on a large scale, although these practices had only placebo effects. In reaction to such malpractice in the first half of the 20th-century science and the young pharmaceutical industry initiated the search for the male hormone. After several detours together with their teams in 1935, Ernst Laqueur (Amsterdam) isolated and Adolf Butenandt (Gdansk), as well as Leopold Ruzicka (Zürich), synthesized testosterone. Since then testosterone has been available for clinical use. However, when given orally, testosterone is inactivated in the liver, so parenteral forms of administration or modifications of the molecule had to be found. Over 85 years the testosterone preparations have been slowly improved so that now physiological serum levels can be achieved.
Isolation and synthesis of testosterone
The craze for such products caused concern about the image of the young field of endocrinology. The famous neurosurgeon, Harvey W Cushing (1869–1939), went so From observation the growth of a cock’s comb under the influence of transplanted testes, Moore et al. (30) in 1929 established the standardized capon comb’s test measuring androgenic activity in square centimeters of comb surface. This first bioassay facilitated the determination of androgenic activity in body products as well as in chemical solutions. In 1930 Loewe and Voss (31) used the biological effects of androgens on the accessory sex organs and developed the ‘cytological regeneration test’ which was based on the regrowth of the seminal vesicle epithelium under the influence of androgenic substances (LoeweVoss-Test). The then still hypothetical male hormone was called ‘Androkinin’. This biological test helped to resolve the question of whether only one or several androgenic steroids existed and, if more than one – which one might be the more potent.
In the dawn of testosterone emerging as a biochemical and marketable entity, and after lengthy negotiation in 1935, Ciba (Switzerland) and Schering-Kahlbaum (Germany), pharmaceutical companies active in the field, started a cooperative effort to inform each other about progress and thus forced their academic protagonists Leopold Ruzicka (1887–1976) at the Technical University of Zürich and Adolf Butenandt (1903–1995) at the then Technical University of Gdansk, to exchange their respective advances, to which the former rivals reluctantly agreed. In 1937 the Ciba-Schering cooperation was extended to include Boehringer (Germany), Chimio Roussel (France), and Organon (The Netherlands) to form a real cartel/syndicate to share knowledge, stake market claims worldwide, and agree on the pricing of the products (1, 21). While economically profitable, this syndicate is also an early example of successful academic-industrial cooperation.
In 1931 Adolf Butenandt, then at the University of Göttingen, isolated the androgenic steroid androsterone (androstan-3α-ol-17-one) from 15,000L of urine provided by young policemen from Berlin and which were processed by Schering to obtain 15mg of this substance. Butenandt considered androsterone the principal androgen (32). Ernst Laqueur (1866–1947) and his group at the University of Amsterdam and at Organon specialized in extracting hormones from animal glands. From 100kg of bull testes, they extracted and isolated 10mg of another androgen, 17β-hydroxy-4-androstene-3one, which they found to be more active than androsterone in biological tests in 1935 (33). They baptized this hormone ‘testosterone’. Although Butenandt liked neither this ‘dreadful’ name nor the competition, in the same year Butenandt and Hanisch (34) at that time at the University of Gdansk, (Fig. 2) as well as Ruzicka and Wettstein (35) in Zurich/Basel (Fig. 3), published the chemical synthesis of testosterone, thus marking the beginning of modern clinical pharmacology of testosterone and male reproductive physiology. For the synthesis of testosterone, Butenandt had started with dehydroandrosterone, while Ruzicka used a degradative approach which he also used for 17alpha-methyltestosterone, the first orally effective testosterone preparation
The close cooperation among the researchers, reinforced by the pharmaceutical companies, may explain why these discoveries were published more or less at the same time. Marius Tausk, one of the former heads of research at Organon who knew the competing protagonists personally, describes the race to testosterone isolation and synthesis very vividly and how the key respective papers were submitted for publication in a short sequence in 1935 (36).
In 1939 Butenandt and Ruzicka received the Nobel Prize for chemistry jointly, Butenandt ‘for his work on sex hormones (estrogen, progesterone, and androsterone – but not for testosterone!) and Ruzicka for his work on polymethylenes and higher terpenes and also not explicitly for testosterone!
Nevertheless, neither laureate could attend the prize ceremony in Stockholm. Butenandt had become director of the Institute for Biochemistry of the KaiserWilhelm-Society in Berlin in 1936; he was prevented by the Nazi regime from accepting the prize since Hitler had forbidden Germans to accept the Nobel Prize after, in 1937, the Nobel Prize for Peace had been awarded to Carl von Ossietzky, a journalist and strong opponent of the regime. In 1949, at the Swedish Consulate in Frankfurt, Butenandt received the Nobel Prize diploma and the medal, but not the money, since according to the statutes, the prize money must be collected within a year.
Incidentally, in 1939 the same indignity was suffered by the Laureate for the Nobel Prize for Medicine, Gerhard Domagk (1894–1964) who worked at the Bayer Company and was honored for his invention of the first clinically used sulfonamide Prontosil®. Domagk was even imprisoned for a few days for accepting the honor and only in 1947 received the Nobel Prize documents from the Swedish King in Stockholm, but – for the same reason as Butenandt – no money. (By the way, Domagk started his academic career between 1925 and 1929 at the University Hospitals in Münster and therefore the author’s institutional street address is named after him.) (37). Back to Butenandt, it should be noted that after the war, his research concentrated on insect hormones and he became president of the Max-Planck-Society (the former Kaiser-Wilhelm-Society), serving from 1960 to 1972.
As Ruzicka was also not able to travel to Stockholm because of turmoil caused by the beginning of World War II, on January 16, 1940 – well within a year – at a special ceremony in Zűrich, the prize was handed over to Ruzicka by the Swedish ambassador in Switzerland, Baron H G Beck-Friis (Fig. 4). After the war had ended, Ruzicka delivered his Nobel Prize lecture on December 12, 1945. In this lecture he explained how research on ‘multimembered rings and higher terpenes guided him to steroids and to testosterone as ‘cholesterol could be regarded as a triterpenoid’ (38). In the 1920s he worked in the perfume industry in Geneva (Switzerland) and Holzminden (Germany) to elucidate the chemical formulas and synthesis of fragrances. His major achievement was the structural analysis and synthesis of the polycyclical ketones such as muscone, the scent in musk pods (preputial glands of the musk deer), civetone from civetts, and santanol from sandalwood, important ingredients in perfumes which before chemical synthesis had to be extracted from their natural sources. In 1929 he became a professor of organic chemistry at the ETH in Zűrich and teamed up with researchers at Ciba in Basel. Ciba was interested in his knowledge of cyclical structures and cooperated with him in the field of triterpenes and steroids, another class of cyclical substances. For the synthesis of testosterone Ruzicka started from cholesterol and used the same degradative approach as for the synthesis of fragrances.
As Ruzicka remarked in autobiographical notes, beyond scientific recognition his research work was also financially rewarding: ‘The patents for the degradative synthesis of testosterone and methyltestosterone earned me during subsequent years an enormous (compared with my professorial standard) amount of money as royalties from Ciba in Basel and Ciba in the USA’. (39). In the year 1939 alone Ciba transferred 56,744 Swiss Francs to Ruzicka as royalties (21). Part of this money was invested in a collection of 17th-century Flemish and Dutch paintings which Ruzicka donated to the Kunsthalle Zürich in 1947 (39) where they form a substantial part of the museum’s inventory
Why Laqueur’s identification of testosterone rather than androsterone as the most important male sex hormone was not recognized by the Nobel Committee in 1939 remains unclear. Laqueur was born in 1880 and grew up near Breslau (Silesia), at that time still in Germany, and received his medical education and degrees in Germany. In 1920 he became a professor of pharmacology at the University of Amsterdam. In 1923 he co-founded Organon located next to the slaughterhouses in Oss (The Netherlands) to extract insulin from pig pancreas. Organon became the first European producer of insulin for the treatment of diabetes. In 1930 Laqueur acquired Dutch nationality. When the Germans invaded The Netherlands in 1940, Laqueur lost his position because of his Jewish background and had to surrender his shares in Organon, but was not further persecuted in contrast to some members of his family.
New syndromes of hypogonadism
It may not have been a coincidence, but a sign of heightened interest in the clinics of hypogonadism that at the same period when testosterone became available for clinical use, that is, when rational treatment became possible, major syndromes of primary and secondary hypogonadism were first described, that is the Klinefelter syndrome in 1942 (40) and the Kallmann syndrome in 1944 (41). Pasqualini and Bur (42) described the fertile eunuch syndrome, characterized by all symptoms of lack of testosterone, but with active spermatogenesis. Also at that time, the symptoms of the aging male were first described systematically, but unfortunately incorrectly termed as ‘male climacteric’ (43), starting a controversial discussion that continues until today. Del Castillo et al. (44) published in1947 the first five cases suffering from Sertoli-cell-only syndrome. Reifenstein (45) first described a syndrome with partial androgen insensitivity (PAIS) that carries his name to date and Morris (46) published the first cases of complete androgen insensitivity (CAIS) as ‘testicular feminization in male pseudohermaphroditism – of course without knowing anything about the androgen receptor or androgen receptor mutations.
Early warning for testosterone
Around the same time, Huggins also posted his warning about testosterone influencing prostate carcinoma (47), which prevailed until quite recently and led to castration as the major treatment of prostate carcinoma, when androgen deprivation therapy (ADT) by GnRH analogs or antiandrogens was introduced instead. Huggins’ statement ‘Cancer of the prostate is activated by androgen injections’ induced a general fear of testosterone, especially among urologists, which prevented testosterone treatment in many patients who might have needed it. Only recently it became clear that neither endogenous serum testosterone levels (48) nor testosterone treatment (49) have an impact on prostate carcinogenesis. Nowadays under careful supervision testosterone treatment is even considered for patients suffering from testosterone deficiency after radical prostatectomy and castration (50).
Development of testosterone preparations for clinical use (1)
Soon after its synthesis, it became clear that, in reasonable doses, testosterone was not effective orally or – as we know it today – would require extremely high doses which were simply not available and/or too expensive. Today we know that the lack of oral effectiveness is due to the inactivation of testosterone by the first-pass effects in the liver. Three approaches were used to overcome this problem:
1. Chemical modification of the steroid molecule,
2. parenteral application and
3. esterification in position 17β of the testosterone molecule.
For a more complete description of the many testosterone preparations and routes of administration, the reader is referred to a review by Behre and Nieschlag (51). A major goal of the efforts to produce new testosterone preparations for clinical use was to optimize the treatment of hypogonadism. Later, when serum levels of testosterone could be determined, an additional goal was to mimic physiological serum testosterone levels as closely as possible (52). As shown in the ensuing text, it took quite a long to reach these goals.
As mentioned above, in 1935 together with testosterone Ruzicka et al. (53) synthesized 17α-methyl-testosterone and demonstrated its oral effectiveness. Since the 17α-configuration protected against degradation in the liver, it soon was well accepted for clinical use (54). However, due to its 17α-structure it was liver toxic, especially under long-term use or at higher doses (55), a feature shared by all 17α substituted androgens. In error some physicians considered liver toxicity a general feature of testosterone preparations, thus making testosterone a dangerous drug. Eventually, at least in Europe, 17α-methyl-testosterone became obsolete for clinical use after the introduction of orally effective testosterone undecanoate in the late 1970s (see below).
As native testosterone proved to be ineffective orally, parenteral routes were explored. Subdermal testosterone pellet implants were the first to be investigated (56) and pellets are still in use today. Their application requires a small operation and harbors the risk of infection and extrusion. However, if enough pellets are implanted, they may provide a substitution for up to half a year and are sporadically still used today (51).
When injected, testosterone has an extremely short half-life of only 10min and as such is not suited for substitution purposes. Therefore, the third possibility of making testosterone clinically effective is esterification at the 17β-hydroxy group of the molecule, making it suitable for intramuscular injection. Testosterone propionate was the first of these esters marketed by Ciba and by Schering in 1936. However, this ester has a short half-life so effective serum levels are reached for only 1–2 days.
Following the propionate ester, testosterone enanthate was synthesized by Junkmann (57) at Schering and marketed as intramuscular Testoviron® Depot injection in 250mg doses, providing substitution for 2–3 weeks (58). However, the pharmacokinetics are characterized by transient supraphysiological peaks for a few days, followed by a slow decline to levels below the lower limit of normal. Although patients do not appreciate these uneven swings in mood, activity, and libido between injections, this remained the major testosterone preparation for the substitution of hypogonadism for half a century and is still used today as a cost-effective alternative to more modern preparations.
Other parenteral routes were tested in the course of the steroid’s history during which testosterone suppositories were marketed by Ferring (59), but yielded rather unpredictable serum levels (58) and are no longer commercially available. A more recent development in this area is bioadhesive buccal testosterone tablets, placed on the gingiva and resulting in effective serum levels if applied twice daily (60). However, due to low patient compliance, they have never penetrated the market. The nasal route has also been explored (61) and has recently been revived for treatment of hypogonadism (62)
From the 1950s to the 1970s, the pharmaceutical industry tried to modify the chemical structure of the molecule in order to disentangle the various effects and produce predominantly erythropoietic, osteogenic, or anabolic steroids. Although more than a thousand of these androgens were synthesized (63), it proved impossible to produce androgens with only one desired effect out of the wide spectrum of testosterone activities. Nevertheless, while some anabolic androgenic steroids (AASs) were clinically used, they disappeared again in the wake of evidence-based medicine. However, they retained a shadow existence for doping in sports and bodybuilding, potentially causing considerable undesired effects (64)
In the 1970s the orally effective testosterone undecanoate, absorbed from the gut via the lymph to avoid the first-pass effect in the liver (65) had been added to the spectrum of testosterone preparations available for replacement therapy. Initial clinical testing revealed that oral testosterone undecanoate was best absorbed with a meal, but the testosterone peaks were short-lived so 3–4 capsules had to be taken during the day in order to produce effective serum levels (66). Oral testosterone undecanoate was introduced to the market worldwide in the late 1970s – except in the USA – and is still in wide use despite rather variable serum testosterone profiles.
In the 1970s the WHO Human Reproduction Program as well as the Population Council of the Rockefeller Foundation had identified male contraception as an unmet need for family planning and as a means against global overpopulation.
Hormonal male contraception based on the combination of testosterone and progestin was at that time – and remains so to date – the most likely candidate for general use. However, the existing testosterone preparations required too frequent applications (for review of clinical trials see (67)). To overcome this deficiency both organizations started programs in search of long-acting testosterone preparations. Under the auspices of WHO, testosterone buciclate was synthesized (68) and identified as a long-acting preparation, well suited for male contraception – and by the same token, also for substitution (69). However, no pharmaceutical company could be persuaded to develop this promising preparation further (70), so in its ensuing clinical trials for male contraception, WHO switched to intramuscular testosterone undecanoate as described below and is now widely used for the treatment of hypogonadism.
Meanwhile, the Population Council had turned to 7α-methyl-19-nortestosterone (MENT) as its preferred androgen for male contraception. This androgen might have the advantage of lacking conversion to DHT and thereby have little effect on the prostate. As MENT has a rather short half-life, it was administered via subdermal Silastic implants, delivering the active substance for a year – or perhaps even longer – thus being well suited for contraception as well as for substitution (71, 72). However, the company interested in further clinical research with this androgen dropped its plans in the wake of being taken over by another company not interested in the male.
In the mid-1990s, transdermal testosterone films applied to the scrotal skin became the first transdermal testosterone preparation in clinical use. Invented by Virgil Place (1924–2012) at ALZA in Palo Alto (CA) and first tested in clinical trials in Münster (73, 74), they showed excellent pharmacokinetic and clinical results and, for the first time, physiological testosterone serum levels could be achieved. Patients were very satisfied with this physiological pharmacokinetic profile, as long-term substitution revealed. However, physicians were reluctant to prescribe a medication to be applied to the scrotum, preferring a subsequently developed non-scrotal testosterone system (75). This, however, caused unpleasant skin reactions as it required an alcoholic enhancer to drive testosterone through the skin (1).
For this reason, the advent of transdermal testosterone gels in 2000 was welcomed for substitution (76). These testosterone-containing gels are applied to the upper arms, shoulders, or abdomen. Those applied in the morning result in physiological serum testosterone levels, almost mimicking the normal diurnal rhythm. Precautions against interpersonal transfer have to be taken, mostly by covering the application sites with a T-shirt. Of the various gels available today, the one with a high 2.5% testosterone concentration can be washed off the skin shortly after application, thereby reducing the danger of contaminating children or women. It has also been tested for scrotal application. Because of the high absorptive capacity of the scrotal skin, only 20% of the gel needed for the non-scrotal application is required, making this form of application economically and ecologically desirable (77), but has not yet been licensed for that purpose.
Finally, in 2004, the intramuscular testosterone undecanoate preparation entered the market and soon achieved great popularity as a real testosterone depot preparation. Testosterone undecanoate, originally provided in oral capsules (see above), had been turned into an injectable preparation by Chinese investigators using tea seed oil as a vehicle. When the author came across it at a meeting in Bejing in 1993 (78), samples were brought to Germany, injected into monkeys, and showed a surprisingly long half-life (79), which could be confirmed in volunteering hypogonadal men who all showed serum levels in the normal range for several weeks (80). When finally a company could be interested in this fascinating preparation, tea seed oil was replaced by castor oil as a vehicle and the injection intervals could be extended to 12 weeks of physiological serum testosterone levels (81, 82). Since 2004, this preparation available in 1000mg ampoules has been licensed in over 100 countries. The latest approval was issued by the FDA in 2014 – however in 750mg doses.
Outlook
Although the effects of testosterone were known for ages, the actual molecule itself was isolated and synthesized only within the last eight decades, that is, in 1935. Since then testosterone has been in clinical use for the substitution of hypogonadal patients. Substitution modalities have been improved slowly by the production of testosterone preparations resulting in physiological serum levels as requested (52). The most recent developments, transdermal testosterone gels, and intramuscular testosterone undecanoate are close to this goal but have not yet reached perfection. Clinical trials for selective androgen receptor modulators (SARMs) have started, but as their goal is selected, testosterone actions such as those required for treatment of sarcopenia or osteoporosis, will not be suited for substitution of hypogonadism, where the full spectrum of testosterone actions is required (83). So far, they seem to be suffering the same fate as androgenic anabolic steroids, even before they have been licensed for clinical use by the drug authorities. As unlicensed substances, they are applied as performance-enhancing substances and for doping. Ultimately, for ideal substitution hope rests on human stem Leydig cells transplanted to hypogonadal patients (84). The goal for these patients – at least those with an intact hypothalamic-pituitary system – would be that the testosterone production required would be provided by the transplanted Leydig cells and would be self-regulated by feedback to LH. These patients would then become independent of exogenous testosterone preparations.
Keep in mind this paper is from 1993and we have come a long way regarding testosterone/DHT and the prostate.
7a-Methyl-Nortestosterone (MENT): The Optimal Androgen For Male Contraception (1993)
Kalyan Sundaram, Narender Kumar and C. Wayne Bardin
Many methods of contraception involve the use of drugs that affect the secretion of hormones essential for reproduction. Oestrogens and progestins have been used for contraception in women as inhibitors of gonadotrophin secretion and ovulation. Similarly, androgens must be used in methods of fertility control for men that block gonadotrophin secretion. Androgen supplementation currently involves large, frequent doses of testosterone esters that are associated with wide fluctuations of plasma testosterone levels. Hence, there Is a need for an androgen preparation that provides appropriate, continuous replacement doses over long periods. To achieve this goal, 7 a-methyl-19. nortestosterone (MENT), a synthetic androgen that Is considerably more potent than testosterone, is suitable. As a consequence, it is feasible to administer this androgen as a substitute for testosterone for 1 year by subdermal implants. Another important feature of MENT is that it does not undergo Sa- reduction In the prostate as does testosterone. As a consequence, a dose of MENT sufficient to maintain normal muscle mass and gonadotrophin secretion will not hyperstimulate the prostate because its action in this organ is not amplified 88 Is that of testosterone. Thus, MENT can be administered to men with the assurance that It will be less prone to cause damage to the prostate than testosterone.
Conclusions: (I) MENT is the first androgen that has a health benefit compared to testosterone; (11) MENT will be promoted as one component of a two-implant system for male contraception, the other component is an implant that All releases an LHRH analog; (lii) MENT has potential uses In patients with a variety of disorders, including hypogonadism, prostatic hyperplasia, and muscle wasting.
Introduction
Some methods of contraception involve the use of drugs that affect the secretion of hormones essential for reproduction. Combined oral contraceptives are used as inhibitors of pituitary gonadotrophins secretion, ovarian hormone secretion, and ovulation. The estrogens and progestins in these contraceptives effectively replace the steroid output of the ovaries that they so efficiently reduce. Methods of fertility control in men that block gonadotrophin secretion and sperm production will also decrease testosterone production. Therefore, androgens will be an essential part of such methods. The most common androgen supplementation involves the administration of large doses of testosterone esters that require frequent injections and that are, in turn, associated with wide fluctuations of plasma testosterone levels. Hence, an androgen preparation is needed that provides appropriate and constant drug delivery over long periods. To achieve this goal, a potent androgen is required that can provide effective treatment for a long period of time with the same mass of drug that is commonly used for testosterone. 7a-methyl-I 9-nortestosterone (MENT) is a synthetic androgen that is considerably more potent than testosterone (Fig. 1). A major advantage of MENT is that it is feasible to administer adequate amounts of this androgen by way of subdermal implants. Another advantage of MENT is that it does not undergo 5a-reduction to a 5a-dihydrosteroid in the prostate as does testosterone. As an element of normal physiology, the action of testosterone is amplified 3-5-fold in the prostate by its conversion to 5a-dihydrotestosterone (DHT). Since MENT avoids this amplification, a dose of this androgen sufficient to maintain normal muscle mass and gonadotrophin secretion will not overstimulate the prostate. Thus, MENT can be administered to men with the assurance that it is less likely to lead to benign prostatic hypertrophy (BPH) than is testosterone. This may be the first androgen that has this particular health benefit.
Because of the high potency of MENT and its acetate (MENTac), adequate amounts of these androgens can be delivered from implants following subdermal placement. Implants are designed to deliver doses that mimic physiological doses of testosterone on muscle and sexual performance. Several studies have shown that the biological activities of MENT and MENTac are the same in a variety of tissues, probably because MENTac is rapidly converted to MENT in vivo. The diffusion rate of MENT from several controlled-release matrices is slow relative to that of MENTac. As a consequence, there is some latitude in the choice of a matrix for implant design. Accordingly, both MENT and MENTac are being examined in several possible implants.
The present review will examine the metabolism and the biological activities of MENT. These observations form the basis of the rationale to recommend MENT as a health-promoting androgen that can be administered by an implant.
Why Is There a Need for a New Androgen?
The goal was to select a new androgen that will be an integral part of any male contraceptive method that depends on the suppression of gonadotropin secretion. Currently, LHRH vaccines as well as LHRH analogs are being investigated as pituitary blocking agents and MENT seems like a good candidate for use with both. In addition, the use of androgen as a primary method of male contraception continues to be under intense scrutiny (1). The androgens most commonly used for these purposes are the various testosterone esters. They are absorbed slowly when injected S.C. or i.m. in an oil depot. Testosterone enanthate (TE) is the most widely used replacement androgen (2, 3). While the clinical effectiveness and safety of TE are well established, it has the disadvantage of requiring i.m. or S.C. administration at 1 -3-week intervals (1, 4). Testosterone cypionate must be injected at similar intervals (5). The pharmacokinetics following the administration of these preparations show that serum testosterone reaches superphysiological levels for 2 or 3 days and then, depending on the frequency of injection, can decline to levels below normal before the next injection (6). Clearly, the need for frequent intramuscular injections and the overdose/ underdose variation is a drawback in the use of these esters. Anadur, a 19-nortestosterone ester must also be given i.m. at 1 -&week intervals at doses of 200 mg (7,8). Testosterone undecanoate, an orally active testosterone ester, is absorbed by the intestinal lymphatics; however, the drug must be taken three times daily to maintain adequate androgen support In addition, the testosterone levels achieved are variable within a subject and among different subjects (9).
Pellet implants, made of compressed testosterone crystals, are cylindrical rods for subdermal implantation (10). They are popular in Australia and the United Kingdom for the treatment of hypogonadism. The implants are inserted subdermally by a minor surgical procedure and last for 4-5 months. Pharmacokinetic studies show that serum testosterone levels reach a high concentration within 1 month and then decline steadily. Serum testosterone levels decline below the normal range before the implant completely dissolves.
To overcome the disadvantages of the highs and lows of the above parenteral preparations, NIH and WHO are investigating long-acting depot preparations. A testosterone ester (testosterone buciclate) has been shown to maintain serum testosterone levels in the normal range for up to 4 months in castrated cynomolgus monkeys after a single intramuscular injection of 40 mg of the ester (11). To achieve a similar goal in man would require the administration of approximately 1 .O g of the ester, a large dose by any measure. In another approach, testosterone is microencapsulated in a biodegradable matrix of lactide/glycolide copolymer that provides effective levels of testosterone for 2-3 months after a single intramuscular injection (1 2). The duration of action of this
In summary, all preparations that use testosterone require the administration of a large mass of the drug. In addition, esters with long side chains add additional bulk to the preparations. MENT, which is 10 times more potent than testosterone, will need to be administered in much smaller doses and thus reduce mass. The estimated daily dose of MENT is expected to be 300-500 pg. Such quantities are easily administered subdermally via sustained release preparations that can be expected to last for 1 year or longer.
In Vitro Metabolism of MENT
In the male reproductive tract and in the skin, testosterone is enzymatically converted via 5a-reductase and the 3-oxidoreductase(s) to androgens with increased activity. These metabolites of testosterone include DHT and the5a-diols. The increased activity of DHT is probably due to its increased affinity to the androgen receptor whereas the increased androgenic action of the Ba-diols is due to oxidation to DHT (1 3). Testosterone can also be aromatized to oestradiol by the enzyme aromatase which is distributed widely in many tissues. The biological role of oestradiol in the male is complex and not fully understood in men. In view of the active products that can be formed from testosterone, it was pertinent to investigate the metabolism of MENT.
5a -Reduction of MENT
The in vitro metabolism of MENT has been investigated in rat liver, ventral prostate, and epididymis (1 4). Radioactively labeled MENT was incubated with tissue homogenates. In liver homogenates three metabolites were identified: 7a-methyl-estr-4-ene-3,7-dione; 7amethyl-5~estrane-3,17/3-diol; and 7a-methyl-3-oxoestr-4-ene-l6,17@-diol. There was no evidence of 5a-dihydro products. In prostate or epididymal homogenates, there was no detectable metabolism of MENT. In parallel investigations, 48% of radiolabelled testosterone was converted to a Ba-reduced product by the prostate and epididymis. We concluded from these observations that MENT does not undergo 5a-reduction, probably because the 7a-methyl group hindered the action of the 5a-reductase. These observations lead to the postulate that compared to testosterone the relative biopotency of MENT on the prostate would be lower than that on muscle.
Aromatization of MENT
Some investigators have postulated that 19-norsteroids cannot be aromatized because of the absence of the /?-methyl group at position-19. To investigate this possibility, 3H-te~to~ter~ne or 3H-MENT were incubated with human placental microsomes in the presence of an NADPH generating system, and the phenolic metabolites were extracted. The extracted metabolites were evaluated by chromatography and by binding to estrogen receptors. These studies indicated that MENT can be metabolized to an oestrogenic compound that is most likely 7amethylestradiol. The conversion of both analogs to estrogens was blocked by an aromatase inhibitor (Table 1).
Basis for the Advantages of MENT
Following the observation that testosterone was converted to DHT in the skin and male reproductive tract, and the realization of its importance in fetal development, it was proposed that testosterone is the physiologically active steroid in many target tissues such as kidney, muscle, pituitary, and brain, since its conversion to DHT could not be demonstrated in vivo in these tissues. Thus, testosterone per se is the androgen that binds to the androgen receptors in these tissues, and the testosterone-receptor complex is the molecular entity that is localized in the nuclei of responsive cells (13). These observations alone provided reason to believe that testosterone is active in many tissues. This postulate, however, was strongly supported by the observations that 5a-reductase inhibitors do not alter the action of testosterone on such tissues (17, 18). In the male reproductive tract (excepting the testis) and sexual skin, testosterone is metabolized to DHT by 5a-reductase (19). Since DHT is 3-5 times more active than testosterone (probably because of its greater affinity for androgen receptors) (20), the action of testosterone is amplified in such tissues. This enhancement of testosterone action is believed to be necessary for the differentiation of the male reproductive tract in the fetus. This conclusion is based on studies of patients with genetically determined Sa-reductase deficiency and on the effects of 5a-reductase inhibitors on androgen-dependent differentiation (21 ).
In adult animals and humans, 5a-reductase inhibitors reduce but do not abolish the action of testosterone on the prostate and other reproductive organs since these inhibitors eliminate the amplification of but not the basal tissue response to testosterone. As a consequence, such agents have been recommended for use in men with BPH by a U.S. FDA advisory committee. Since 5areductase is also present in sexual skin, these inhibitors may also retard beard growth and reduce androgen-dependent hair loss from the scalp. Other possible biological consequences of the blockade of this enzyme in adults are not evident from studies to date but are being extensively evaluated as new inhibitors are further examined in men. Thus, there is considerable evidence to indicate that the action of testosterone is amplified in the prostate and other reproductive organs. However, at present, there is no known physiological need for amplification of the action of testosterone in adults. If this is the case then MENT should be able to provide suitable androgen replacement in hypogonadal men. The goal of treatment would be to select a dose that would maintain the metabolic and behavioral effects of testosterone without hyperstimulation of the prostate.
That there is no known physiological need for amplification of testosterone action in adults suggests that chronic use of 5a-reductase inhibitors could prevent BPH and possibly prostate cancer. Although this postulate is attractive, the potent effects of 5a-reductase inhibitors on fetal sexual differentiation and the possible transfer of these inhibitors from male to female in semen may preclude their widespread prolonged use in healthy men. Therefore, 5a-reductase inhibitors can be recommended for use in men with established prostatic hyperplasia rather than as an agent that will prevent its occurrence. Based on these considerations, we propose that an alternative approach that could be used in healthy men is to suppress testosterone secretion with an LHRH analog and then use MENT to maintain libido and the metabolic effects of testosterone. Replacement with MENT would be analogous to treatment with a 5a-reductase inhibitor since MENT cannot be reduced by 5a-reductase. If it can be demonstrated that an implant system that delivers LHRH analog plus MENT can safely be used for contraception in men then similar implants could also be used to limit the development of BPH.
We conclude that the use of MENT instead of testosterone for androgen replacement in hypogonadal men and as a component of a male contraceptive could have health-promoting effects by reducing the occurrence of prostatic disease.
7α-Methyl-19-nortestosterone (MENTR): the Population Council's contribution to research on male contraception and treatment of hypogonadism (2013)
Eberhard Nieschlaga,⁎, Narender Kumar b , Régine Sitruk-Ware
Abstract Testosterone is an essential part of all regimens for hormonal male contraception tested to date. Initial efficacy trials revealed that the half-life of the testosterone preparations available at that time was too short to be used for male contraception. The ensuing search for long-acting preparations yielded testosterone buciclate and undecanoate as well as 7α-methyl-19-nortestosterone (MENT). The following description of the principle of male hormonal contraception and the efficacy trials performed to date, the systematic development of MENT for substitution of male hypogonadism, and use in male contraception by the Population Council is reviewed here.
1. Introduction
Men are increasingly expected and willing to share the responsibility for family planning by using contraceptive methods [1]. However, traditional male methods of contraception such as periodic abstinence or coitus interruptus are associated with a relatively high rate of unwanted pregnancies as well as disturbances in sexual activity. Condoms are the oldest barrier method available, but when using condoms, conception rates remain relatively high, with 12/ 100 couples conceiving during the first year of use. Nevertheless, condom use has increased since the beginning of the AIDS epidemic, but more for protection from AIDS infection and other sexually transmitted diseases than for contraceptive purposes. Vasectomy is a safe and surgically relatively simple method for male contraception. The rate of unwanted pregnancies after vasectomy is less than 1%. The drawback of vasectomy is that it is not easily reversible. Achieving fatherhood after vasectomy requires either surgical refertilization or sperm aspiration from the epididymis or testicular sperm extraction and intracytoplasmic sperm injection into the ovum. Only about 50% of these men will ultimately become fathers.
Considering these disadvantages of the traditional male contraceptive methods mentioned above, the prerequisites for an ideal pharmacologic male contraceptive become clear, they should [2]:
• be applied independently of the sexual act,
• be acceptable for both partners,
• not interfere with libido, potency, or sexual activity,
• have neither short- nor long-term toxic side effects,
• have no impact on eventual offspring,
• be rapidly effective and fully reversible and
• be as safe and effective as comparable female methods.
Of all the different experimental approaches to pharmacological methods for male contraception tested so far, hormonal methods come closest to fulfilling the criteria set out above. The endocrine feedback mechanism operating between the hypothalamus, pituitary, and testes is the basis on which hormonal approaches to male contraception rest. Their goal is to suppress spermatogenesis and to reduce sperm concentration, if possible, to azoospermia or at least to a sperm concentration low enough to provide contraceptive protection to a degree at least as good as generally accepted female contraceptive methods.
Sperm production and secretion of testicular testosterone are so closely interwoven [3] that it has remained impossible to interrupt spermatogenesis by hormonal means without inhibiting androgen production. Inhibition of follicle-stimulating hormone (FSH) alone, e.g., by active immunization against FSH, leads to a reduction of sperm concentration but not to azoospermia, as monkey studies have shown [4]. Suppression of both FSH and luteinizing hormone (LH) will indeed lead to azoospermia, but will also induce symptoms of androgen deficiency affecting libido, erectile function, male behavior, and general metabolic processes (including erythropoiesis, protein, mineral, and bone metabolism). For this reason, inhibition of gonadotropins will always necessitate androgen administration [5]. Therefore, the principle of hormonal male contraception consists of [2]:
1. suppression of LH and FSH,
2. depletion of intratesticular testosterone and atrophy of spermatogenesis and
3. the substitution of peripheral testosterone to maintain androgenicity.
Testosterone itself is the first choice for hormonal male contraception as it simultaneously suppresses gonadotropins and maintains androgenicity, and indeed, testosterone alone was the first hormone tested for male contraception and has remained part of any steroid combination to date [5].
3. Development of MENTR for the treatment of hypogonadism
From the initial unsuccessful efficacy trial performed by the Population Council [7] and further preclinical and clinical investigations (e.g., [27]), it became clear that constant suppression of gonadotropins would be required to achieve or at least approach azoospermia in the semen of the volunteers. As the existing depot testosterone preparations at that time (i.e., testosterone enanthate and cypionate) had to be injected too frequently to be applicable in male contraception, the search for suitable depot formulation began. At that time, the Population Council had developed NorplantR as a long-acting female contraceptive based on levonorgestrel delivered from subcutaneous Silastic implants lasting for 7 years [28]. As this proved to be a very successful method for steroid delivery, the possible use of implants for testosterone delivery was obvious. However, a year's supply of testosterone for male contraception would be in the gram range and thus would have exceeded the capacity of a practical implant. Therefore, for implant delivery, a more potent androgen requiring less volume was needed. In addition, the search was made for an androgen that would not be a substrate for the 5α-reductase enzyme in order to spare the prostate from the androgenic effect. Several molecules were screened, and the final choice was MENTR.
MENTR had been synthesized by the Upjohn Company in the early 1960s as an androgenic–anabolic steroid for potential use in oncological therapy. In the immature castrated rat, MENTR had shown an apparently five times higher potency than testosterone (propionate) with regard to levator ani and seminal vesicle weights [29] and thus appeared to be an appropriate candidate for male contraception [30] as well as for androgen substitution in hypogonadal men [31]. Under C.W. Bardin's and K. Sundaram's aegis, systematic development of MENTR for clinical purposes was started. The necessary toxicology was undertaken, and a radioimmunoassay for MENTR to be used in pharmacokinetic studies in animals and humans was established [32,33]. In rats and later in humans, the high androgenic potency of MENTR could be confirmed [34]. As preclinical studies ascertained that MENTR was acceptable for human use, the manufacturing of SilasticR implants was initiated. First, implants with a length of 4.5 cm and a diameter of 2.7 cm containing 112 mg MENTR acetate were produced. When two or four of these rods were implanted subcutaneously in volunteers, MENTR serum levels ranged between 1 and 3 nmol/L, and LH and FSH were suppressed in a dose-dependent fashion during the 4-week trial period [35,36].
In an ensuing study in 16 hypogonadal men using one or two implants of slightly higher potency for 24 weeks, the suitability of MENTR for substitution purposes was demonstrated, especially in regard to sexual functions, but two special features emerged [37]. As shown earlier in monkeys [38], MENTR appeared to have a prostate-sparing effect in men since the prostate did not grow to the extent expected under full testosterone substitution. This effect was attributed to the fact that MENTR is not converted to 5αdihydrotestosterone and therefore might have less effect on prostate growth. However, in the same study, it was also observed that bone density in the hypogonadal men treated with MENTR did not reach the same level as in the control group treated with testosterone enanthate. This could indicate that the MENTR dose delivered in the study was not high enough for full androgenicity and triggered a thorough investigation into the effect of MENTR on bones. In the aged male castrated rat model, it was demonstrated that MENTR was well suited to restore fully normal bone structure if administered at the appropriate dose [39]. The supposed “tissue selectivity” of MENTR [37] in regard to prostate and bones could reflect the phenomenon of different threshold levels for the effects of testosterone (and androgens in general) for fully normal functions of tissues and organs as reflected by the occurrence of specific symptoms at specific testosterone levels when lowering testosterone levels in testosterone-treated hypogonadal men [40,41].
Overall, using the proper dose, MENTR appears to be well suited for the substitution of male hypogonadism. For this purpose, Schering Pharma further developed MENTR into a transdermal gel preparation by adding a fluor atom in position 11 (11-fluoro-7α-methyl-19-nortestosterone= eF-MENTR). In the phase, I study, effectiveness in treating sexual symptoms of hypogonadal men and reduced stimulation of the prostate could be demonstrated [42]. Despite these promising results, when Bayer acquired Schering to become Bayer HealthCare, the company decided to discontinue its research in this field. Therefore, the future of MENTR and eF-MENTR gels for the treatment of hypogonadism is uncertain at this stage.
5. Outlook
As this article shows, neither the development of MENTR in particular nor hormonal male contraception research, in general, has yet resulted in a product ready for licensing and application. However, the occasion of the 100th meeting of the Population Council's International Committee on Contraception Research provides an opportunity to pause and take stock of the 40-year history of research in hormonal male contraception.
Although the principle of hormonal male contraception has been proven, it appears to be extremely difficult to work out details of the steroid combination to be used and to bring it to the consumer. Without the input of the pharmaceutical industry, it will be impossible to complete the final steps in this development. However, the reluctance of the pharmaceutical industry to enter the field of male contraception has been additionally reinforced by the WHO decision to suspend the TU/NETE efficacy study. A concentrated effort by investigators, donor organizations, and politicians will be required to bring the industry back into the field or to take the lead in such development.
Although opinion polls among possible consumers indicate a willingness to use such methods and despite the keen interest of the media in male contraception, there is no strong urge on the part of society to develop male contraceptives. Research for female contraceptives before the arrival of the “pill” was driven by large segments of the female population fighting for gender equality and freedom from reproductive burdens. Although many men would now be willing to use a hormonal male contraceptive, there is no real force behind this intention. Men (and women) are not taking to the streets to rally for male contraception. There is a decisive gender difference between men and women in the perception of contraception. For women, contraception means personally avoiding pregnancy with all its medical, social, and economic implications, including the threat of death from childbearing. In contrast, for men, contraception is more a rational issue regarding respect for the partner and avoiding financial, social, and legal obligations of fatherhood. However, the time can be foreseen when even this rational approach may result in popular demand for male contraception, be it for the purpose of sharing responsibility for family planning by both sexes, be it for a contribution to reducing overpopulation and maintaining an ecological balance or be it for men's desire to regain reproductive power, a motive not so acceptable to advocacy groups. Until this time comes, the endurance and perseverance of organizations such as the Population Council are of utmost importance to maintain the field of male contraception research be it on an underpowered level due to lack of sufficient funding.
Attachments
Wow that's going to take meYou need to post your most recent labs.
Weare flying blind here.
Need to know where your trough TT, FT, and estradiol sit let alone RBCs/hemoglobin/hematocrit.
Hopefully, you tested using the most accurate assays TT/estradiol (LC/MS-MS) and FT (Equilibrium Dialysis or Ultrafiltration).
You have highish SHBG so it is critical that you tested using an accurate assay.
Methandrostenolone could never replace testosterone let alone it is not something that one would use long-term due to the compound being c-17 alpha alkylated which is known to stress the liver.
The use of AAS 17α-alkylated orals such as stanozolol, oxandrolone, methyltestosterone, methandrostenolone, oxymetholone, and fluoxymesterone are notorious for driving down HDL, increasing LDL, stressing the liver and hammering down SHBG.
Even then the dose/duration of use will play a big role.
Highly doubtful you are going to run into any serious liver damage from using therapeutic does (oxandrolone/stanazolol) let alone low doses of any other c-17 alpha alkylated orals from short-term use.
No AAS would be a substitution for testosterone.
If anything there may be some merit in using 7α-methyl-19-nortestosterone (MENT) which appears to be an appropriate candidate for androgen substitution in hypogonadal men as it possesses high androgenic potency and aromatizes to 7amethylestradiol.
Mind you it is not converted to DHT let alone the studies done were on a small number of patients who were using extremely low doses (subcutaneous implants/transdermal gel) and they were not long-term (>1 yr).
Hard to say what impact this would have as a sole replacement long-term especially when it comes to libido/brain chemistry.
If you feel comfortable giving it a shot go nuts!
The main reason testosterone is used for replacement therapy over nandrolone let alone any other AAS is that testosterone drugs provide a hormone that is already produced in the body.
Let alone metabolites estradiol and DHT are needed in healthy amounts to experience the full spectrum of testosterones beneficial effects on (cardiovascular health, brain health, libido, erectile function, bone health, tendon health, immune system, lipids, and body composition).
*Natural testosterone is viewed as the best androgen for substitution in hypogonadal men. The reason behind the selection is that testosterone can be converted to DHT and E2, thus developing the full spectrum of testosterone activities in long-term substitution
*Preparations of native testosterone or its esters (aromatizable T) should be used for TTh
The history of discovery, synthesis, and development of testosterone for clinical use (2015)
Eberhard Nieschlag and Susan Nieschlag
Abstract
As the most important male hormone, testosterone has an impact on almost all organs and body functions. The biological effects of testosterone and the testes have been known since antiquity, long before testosterone was identified as an active agent. Practical applications of this knowledge were the castration of males to produce obedient servants, for punishment, for the preservation of the prepubertal soprano voice, and even for the treatment of diseases. Testes were used in organotherapy and transplanted as a treatment for symptoms of hypogonadism on a large scale, although these practices had only placebo effects. In reaction to such malpractice in the first half of the 20th-century science and the young pharmaceutical industry initiated the search for the male hormone. After several detours together with their teams in 1935, Ernst Laqueur (Amsterdam) isolated and Adolf Butenandt (Gdansk), as well as Leopold Ruzicka (Zürich), synthesized testosterone. Since then testosterone has been available for clinical use. However, when given orally, testosterone is inactivated in the liver, so parenteral forms of administration or modifications of the molecule had to be found. Over 85 years the testosterone preparations have been slowly improved so that now physiological serum levels can be achieved.
Isolation and synthesis of testosterone
The craze for such products caused concern about the image of the young field of endocrinology. The famous neurosurgeon, Harvey W Cushing (1869–1939), went so From observation the growth of a cock’s comb under the influence of transplanted testes, Moore et al. (30) in 1929 established the standardized capon comb’s test measuring androgenic activity in square centimeters of comb surface. This first bioassay facilitated the determination of androgenic activity in body products as well as in chemical solutions. In 1930 Loewe and Voss (31) used the biological effects of androgens on the accessory sex organs and developed the ‘cytological regeneration test’ which was based on the regrowth of the seminal vesicle epithelium under the influence of androgenic substances (LoeweVoss-Test). The then still hypothetical male hormone was called ‘Androkinin’. This biological test helped to resolve the question of whether only one or several androgenic steroids existed and, if more than one – which one might be the more potent.
In the dawn of testosterone emerging as a biochemical and marketable entity, and after lengthy negotiation in 1935, Ciba (Switzerland) and Schering-Kahlbaum (Germany), pharmaceutical companies active in the field, started a cooperative effort to inform each other about progress and thus forced their academic protagonists Leopold Ruzicka (1887–1976) at the Technical University of Zürich and Adolf Butenandt (1903–1995) at the then Technical University of Gdansk, to exchange their respective advances, to which the former rivals reluctantly agreed. In 1937 the Ciba-Schering cooperation was extended to include Boehringer (Germany), Chimio Roussel (France), and Organon (The Netherlands) to form a real cartel/syndicate to share knowledge, stake market claims worldwide, and agree on the pricing of the products (1, 21). While economically profitable, this syndicate is also an early example of successful academic-industrial cooperation.
In 1931 Adolf Butenandt, then at the University of Göttingen, isolated the androgenic steroid androsterone (androstan-3α-ol-17-one) from 15,000L of urine provided by young policemen from Berlin and which were processed by Schering to obtain 15mg of this substance. Butenandt considered androsterone the principal androgen (32). Ernst Laqueur (1866–1947) and his group at the University of Amsterdam and at Organon specialized in extracting hormones from animal glands. From 100kg of bull testes, they extracted and isolated 10mg of another androgen, 17β-hydroxy-4-androstene-3one, which they found to be more active than androsterone in biological tests in 1935 (33). They baptized this hormone ‘testosterone’. Although Butenandt liked neither this ‘dreadful’ name nor the competition, in the same year Butenandt and Hanisch (34) at that time at the University of Gdansk, (Fig. 2) as well as Ruzicka and Wettstein (35) in Zurich/Basel (Fig. 3), published the chemical synthesis of testosterone, thus marking the beginning of modern clinical pharmacology of testosterone and male reproductive physiology. For the synthesis of testosterone, Butenandt had started with dehydroandrosterone, while Ruzicka used a degradative approach which he also used for 17alpha-methyltestosterone, the first orally effective testosterone preparation
The close cooperation among the researchers, reinforced by the pharmaceutical companies, may explain why these discoveries were published more or less at the same time. Marius Tausk, one of the former heads of research at Organon who knew the competing protagonists personally, describes the race to testosterone isolation and synthesis very vividly and how the key respective papers were submitted for publication in a short sequence in 1935 (36).
In 1939 Butenandt and Ruzicka received the Nobel Prize for chemistry jointly, Butenandt ‘for his work on sex hormones (estrogen, progesterone, and androsterone – but not for testosterone!) and Ruzicka for his work on polymethylenes and higher terpenes and also not explicitly for testosterone!
Nevertheless, neither laureate could attend the prize ceremony in Stockholm. Butenandt had become director of the Institute for Biochemistry of the KaiserWilhelm-Society in Berlin in 1936; he was prevented by the Nazi regime from accepting the prize since Hitler had forbidden Germans to accept the Nobel Prize after, in 1937, the Nobel Prize for Peace had been awarded to Carl von Ossietzky, a journalist and strong opponent of the regime. In 1949, at the Swedish Consulate in Frankfurt, Butenandt received the Nobel Prize diploma and the medal, but not the money, since according to the statutes, the prize money must be collected within a year.
Incidentally, in 1939 the same indignity was suffered by the Laureate for the Nobel Prize for Medicine, Gerhard Domagk (1894–1964) who worked at the Bayer Company and was honored for his invention of the first clinically used sulfonamide Prontosil®. Domagk was even imprisoned for a few days for accepting the honor and only in 1947 received the Nobel Prize documents from the Swedish King in Stockholm, but – for the same reason as Butenandt – no money. (By the way, Domagk started his academic career between 1925 and 1929 at the University Hospitals in Münster and therefore the author’s institutional street address is named after him.) (37). Back to Butenandt, it should be noted that after the war, his research concentrated on insect hormones and he became president of the Max-Planck-Society (the former Kaiser-Wilhelm-Society), serving from 1960 to 1972.
As Ruzicka was also not able to travel to Stockholm because of turmoil caused by the beginning of World War II, on January 16, 1940 – well within a year – at a special ceremony in Zűrich, the prize was handed over to Ruzicka by the Swedish ambassador in Switzerland, Baron H G Beck-Friis (Fig. 4). After the war had ended, Ruzicka delivered his Nobel Prize lecture on December 12, 1945. In this lecture he explained how research on ‘multimembered rings and higher terpenes guided him to steroids and to testosterone as ‘cholesterol could be regarded as a triterpenoid’ (38). In the 1920s he worked in the perfume industry in Geneva (Switzerland) and Holzminden (Germany) to elucidate the chemical formulas and synthesis of fragrances. His major achievement was the structural analysis and synthesis of the polycyclical ketones such as muscone, the scent in musk pods (preputial glands of the musk deer), civetone from civetts, and santanol from sandalwood, important ingredients in perfumes which before chemical synthesis had to be extracted from their natural sources. In 1929 he became a professor of organic chemistry at the ETH in Zűrich and teamed up with researchers at Ciba in Basel. Ciba was interested in his knowledge of cyclical structures and cooperated with him in the field of triterpenes and steroids, another class of cyclical substances. For the synthesis of testosterone Ruzicka started from cholesterol and used the same degradative approach as for the synthesis of fragrances.
As Ruzicka remarked in autobiographical notes, beyond scientific recognition his research work was also financially rewarding: ‘The patents for the degradative synthesis of testosterone and methyltestosterone earned me during subsequent years an enormous (compared with my professorial standard) amount of money as royalties from Ciba in Basel and Ciba in the USA’. (39). In the year 1939 alone Ciba transferred 56,744 Swiss Francs to Ruzicka as royalties (21). Part of this money was invested in a collection of 17th-century Flemish and Dutch paintings which Ruzicka donated to the Kunsthalle Zürich in 1947 (39) where they form a substantial part of the museum’s inventory
Why Laqueur’s identification of testosterone rather than androsterone as the most important male sex hormone was not recognized by the Nobel Committee in 1939 remains unclear. Laqueur was born in 1880 and grew up near Breslau (Silesia), at that time still in Germany, and received his medical education and degrees in Germany. In 1920 he became a professor of pharmacology at the University of Amsterdam. In 1923 he co-founded Organon located next to the slaughterhouses in Oss (The Netherlands) to extract insulin from pig pancreas. Organon became the first European producer of insulin for the treatment of diabetes. In 1930 Laqueur acquired Dutch nationality. When the Germans invaded The Netherlands in 1940, Laqueur lost his position because of his Jewish background and had to surrender his shares in Organon, but was not further persecuted in contrast to some members of his family.
New syndromes of hypogonadism
It may not have been a coincidence, but a sign of heightened interest in the clinics of hypogonadism that at the same period when testosterone became available for clinical use, that is, when rational treatment became possible, major syndromes of primary and secondary hypogonadism were first described, that is the Klinefelter syndrome in 1942 (40) and the Kallmann syndrome in 1944 (41). Pasqualini and Bur (42) described the fertile eunuch syndrome, characterized by all symptoms of lack of testosterone, but with active spermatogenesis. Also at that time, the symptoms of the aging male were first described systematically, but unfortunately incorrectly termed as ‘male climacteric’ (43), starting a controversial discussion that continues until today. Del Castillo et al. (44) published in1947 the first five cases suffering from Sertoli-cell-only syndrome. Reifenstein (45) first described a syndrome with partial androgen insensitivity (PAIS) that carries his name to date and Morris (46) published the first cases of complete androgen insensitivity (CAIS) as ‘testicular feminization in male pseudohermaphroditism – of course without knowing anything about the androgen receptor or androgen receptor mutations.
Early warning for testosterone
Around the same time, Huggins also posted his warning about testosterone influencing prostate carcinoma (47), which prevailed until quite recently and led to castration as the major treatment of prostate carcinoma, when androgen deprivation therapy (ADT) by GnRH analogs or antiandrogens was introduced instead. Huggins’ statement ‘Cancer of the prostate is activated by androgen injections’ induced a general fear of testosterone, especially among urologists, which prevented testosterone treatment in many patients who might have needed it. Only recently it became clear that neither endogenous serum testosterone levels (48) nor testosterone treatment (49) have an impact on prostate carcinogenesis. Nowadays under careful supervision testosterone treatment is even considered for patients suffering from testosterone deficiency after radical prostatectomy and castration (50).
Development of testosterone preparations for clinical use (1)
Soon after its synthesis, it became clear that, in reasonable doses, testosterone was not effective orally or – as we know it today – would require extremely high doses which were simply not available and/or too expensive. Today we know that the lack of oral effectiveness is due to the inactivation of testosterone by the first-pass effects in the liver. Three approaches were used to overcome this problem:
1. Chemical modification of the steroid molecule,
2. parenteral application and
3. esterification in position 17β of the testosterone molecule.
For a more complete description of the many testosterone preparations and routes of administration, the reader is referred to a review by Behre and Nieschlag (51). A major goal of the efforts to produce new testosterone preparations for clinical use was to optimize the treatment of hypogonadism. Later, when serum levels of testosterone could be determined, an additional goal was to mimic physiological serum testosterone levels as closely as possible (52). As shown in the ensuing text, it took quite a long to reach these goals.
As mentioned above, in 1935 together with testosterone Ruzicka et al. (53) synthesized 17α-methyl-testosterone and demonstrated its oral effectiveness. Since the 17α-configuration protected against degradation in the liver, it soon was well accepted for clinical use (54). However, due to its 17α-structure it was liver toxic, especially under long-term use or at higher doses (55), a feature shared by all 17α substituted androgens. In error some physicians considered liver toxicity a general feature of testosterone preparations, thus making testosterone a dangerous drug. Eventually, at least in Europe, 17α-methyl-testosterone became obsolete for clinical use after the introduction of orally effective testosterone undecanoate in the late 1970s (see below).
As native testosterone proved to be ineffective orally, parenteral routes were explored. Subdermal testosterone pellet implants were the first to be investigated (56) and pellets are still in use today. Their application requires a small operation and harbors the risk of infection and extrusion. However, if enough pellets are implanted, they may provide a substitution for up to half a year and are sporadically still used today (51).
When injected, testosterone has an extremely short half-life of only 10min and as such is not suited for substitution purposes. Therefore, the third possibility of making testosterone clinically effective is esterification at the 17β-hydroxy group of the molecule, making it suitable for intramuscular injection. Testosterone propionate was the first of these esters marketed by Ciba and by Schering in 1936. However, this ester has a short half-life so effective serum levels are reached for only 1–2 days.
Following the propionate ester, testosterone enanthate was synthesized by Junkmann (57) at Schering and marketed as intramuscular Testoviron® Depot injection in 250mg doses, providing substitution for 2–3 weeks (58). However, the pharmacokinetics are characterized by transient supraphysiological peaks for a few days, followed by a slow decline to levels below the lower limit of normal. Although patients do not appreciate these uneven swings in mood, activity, and libido between injections, this remained the major testosterone preparation for the substitution of hypogonadism for half a century and is still used today as a cost-effective alternative to more modern preparations.
Other parenteral routes were tested in the course of the steroid’s history during which testosterone suppositories were marketed by Ferring (59), but yielded rather unpredictable serum levels (58) and are no longer commercially available. A more recent development in this area is bioadhesive buccal testosterone tablets, placed on the gingiva and resulting in effective serum levels if applied twice daily (60). However, due to low patient compliance, they have never penetrated the market. The nasal route has also been explored (61) and has recently been revived for treatment of hypogonadism (62)
From the 1950s to the 1970s, the pharmaceutical industry tried to modify the chemical structure of the molecule in order to disentangle the various effects and produce predominantly erythropoietic, osteogenic, or anabolic steroids. Although more than a thousand of these androgens were synthesized (63), it proved impossible to produce androgens with only one desired effect out of the wide spectrum of testosterone activities. Nevertheless, while some anabolic androgenic steroids (AASs) were clinically used, they disappeared again in the wake of evidence-based medicine. However, they retained a shadow existence for doping in sports and bodybuilding, potentially causing considerable undesired effects (64)
In the 1970s the orally effective testosterone undecanoate, absorbed from the gut via the lymph to avoid the first-pass effect in the liver (65) had been added to the spectrum of testosterone preparations available for replacement therapy. Initial clinical testing revealed that oral testosterone undecanoate was best absorbed with a meal, but the testosterone peaks were short-lived so 3–4 capsules had to be taken during the day in order to produce effective serum levels (66). Oral testosterone undecanoate was introduced to the market worldwide in the late 1970s – except in the USA – and is still in wide use despite rather variable serum testosterone profiles.
In the 1970s the WHO Human Reproduction Program as well as the Population Council of the Rockefeller Foundation had identified male contraception as an unmet need for family planning and as a means against global overpopulation.
Hormonal male contraception based on the combination of testosterone and progestin was at that time – and remains so to date – the most likely candidate for general use. However, the existing testosterone preparations required too frequent applications (for review of clinical trials see (67)). To overcome this deficiency both organizations started programs in search of long-acting testosterone preparations. Under the auspices of WHO, testosterone buciclate was synthesized (68) and identified as a long-acting preparation, well suited for male contraception – and by the same token, also for substitution (69). However, no pharmaceutical company could be persuaded to develop this promising preparation further (70), so in its ensuing clinical trials for male contraception, WHO switched to intramuscular testosterone undecanoate as described below and is now widely used for the treatment of hypogonadism.
Meanwhile, the Population Council had turned to 7α-methyl-19-nortestosterone (MENT) as its preferred androgen for male contraception. This androgen might have the advantage of lacking conversion to DHT and thereby have little effect on the prostate. As MENT has a rather short half-life, it was administered via subdermal Silastic implants, delivering the active substance for a year – or perhaps even longer – thus being well suited for contraception as well as for substitution (71, 72). However, the company interested in further clinical research with this androgen dropped its plans in the wake of being taken over by another company not interested in the male.
In the mid-1990s, transdermal testosterone films applied to the scrotal skin became the first transdermal testosterone preparation in clinical use. Invented by Virgil Place (1924–2012) at ALZA in Palo Alto (CA) and first tested in clinical trials in Münster (73, 74), they showed excellent pharmacokinetic and clinical results and, for the first time, physiological testosterone serum levels could be achieved. Patients were very satisfied with this physiological pharmacokinetic profile, as long-term substitution revealed. However, physicians were reluctant to prescribe a medication to be applied to the scrotum, preferring a subsequently developed non-scrotal testosterone system (75). This, however, caused unpleasant skin reactions as it required an alcoholic enhancer to drive testosterone through the skin (1).
For this reason, the advent of transdermal testosterone gels in 2000 was welcomed for substitution (76). These testosterone-containing gels are applied to the upper arms, shoulders, or abdomen. Those applied in the morning result in physiological serum testosterone levels, almost mimicking the normal diurnal rhythm. Precautions against interpersonal transfer have to be taken, mostly by covering the application sites with a T-shirt. Of the various gels available today, the one with a high 2.5% testosterone concentration can be washed off the skin shortly after application, thereby reducing the danger of contaminating children or women. It has also been tested for scrotal application. Because of the high absorptive capacity of the scrotal skin, only 20% of the gel needed for the non-scrotal application is required, making this form of application economically and ecologically desirable (77), but has not yet been licensed for that purpose.
Finally, in 2004, the intramuscular testosterone undecanoate preparation entered the market and soon achieved great popularity as a real testosterone depot preparation. Testosterone undecanoate, originally provided in oral capsules (see above), had been turned into an injectable preparation by Chinese investigators using tea seed oil as a vehicle. When the author came across it at a meeting in Bejing in 1993 (78), samples were brought to Germany, injected into monkeys, and showed a surprisingly long half-life (79), which could be confirmed in volunteering hypogonadal men who all showed serum levels in the normal range for several weeks (80). When finally a company could be interested in this fascinating preparation, tea seed oil was replaced by castor oil as a vehicle and the injection intervals could be extended to 12 weeks of physiological serum testosterone levels (81, 82). Since 2004, this preparation available in 1000mg ampoules has been licensed in over 100 countries. The latest approval was issued by the FDA in 2014 – however in 750mg doses.
Outlook
Although the effects of testosterone were known for ages, the actual molecule itself was isolated and synthesized only within the last eight decades, that is, in 1935. Since then testosterone has been in clinical use for the substitution of hypogonadal patients. Substitution modalities have been improved slowly by the production of testosterone preparations resulting in physiological serum levels as requested (52). The most recent developments, transdermal testosterone gels, and intramuscular testosterone undecanoate are close to this goal but have not yet reached perfection. Clinical trials for selective androgen receptor modulators (SARMs) have started, but as their goal is selected, testosterone actions such as those required for treatment of sarcopenia or osteoporosis, will not be suited for substitution of hypogonadism, where the full spectrum of testosterone actions is required (83). So far, they seem to be suffering the same fate as androgenic anabolic steroids, even before they have been licensed for clinical use by the drug authorities. As unlicensed substances, they are applied as performance-enhancing substances and for doping. Ultimately, for ideal substitution hope rests on human stem Leydig cells transplanted to hypogonadal patients (84). The goal for these patients – at least those with an intact hypothalamic-pituitary system – would be that the testosterone production required would be provided by the transplanted Leydig cells and would be self-regulated by feedback to LH. These patients would then become independent of exogenous testosterone preparations.
Keep in mind this paper is from 1993and we have come a long way regarding testosterone/DHT and the prostate.
7a-Methyl-Nortestosterone (MENT): The Optimal Androgen For Male Contraception (1993)
Kalyan Sundaram, Narender Kumar and C. Wayne Bardin
Many methods of contraception involve the use of drugs that affect the secretion of hormones essential for reproduction. Oestrogens and progestins have been used for contraception in women as inhibitors of gonadotrophin secretion and ovulation. Similarly, androgens must be used in methods of fertility control for men that block gonadotrophin secretion. Androgen supplementation currently involves large, frequent doses of testosterone esters that are associated with wide fluctuations of plasma testosterone levels. Hence, there Is a need for an androgen preparation that provides appropriate, continuous replacement doses over long periods. To achieve this goal, 7 a-methyl-19. nortestosterone (MENT), a synthetic androgen that Is considerably more potent than testosterone, is suitable. As a consequence, it is feasible to administer this androgen as a substitute for testosterone for 1 year by subdermal implants. Another important feature of MENT is that it does not undergo Sa- reduction In the prostate as does testosterone. As a consequence, a dose of MENT sufficient to maintain normal muscle mass and gonadotrophin secretion will not hyperstimulate the prostate because its action in this organ is not amplified 88 Is that of testosterone. Thus, MENT can be administered to men with the assurance that It will be less prone to cause damage to the prostate than testosterone.
Conclusions: (I) MENT is the first androgen that has a health benefit compared to testosterone; (11) MENT will be promoted as one component of a two-implant system for male contraception, the other component is an implant that All releases an LHRH analog; (lii) MENT has potential uses In patients with a variety of disorders, including hypogonadism, prostatic hyperplasia, and muscle wasting.
Introduction
Some methods of contraception involve the use of drugs that affect the secretion of hormones essential for reproduction. Combined oral contraceptives are used as inhibitors of pituitary gonadotrophins secretion, ovarian hormone secretion, and ovulation. The estrogens and progestins in these contraceptives effectively replace the steroid output of the ovaries that they so efficiently reduce. Methods of fertility control in men that block gonadotrophin secretion and sperm production will also decrease testosterone production. Therefore, androgens will be an essential part of such methods. The most common androgen supplementation involves the administration of large doses of testosterone esters that require frequent injections and that are, in turn, associated with wide fluctuations of plasma testosterone levels. Hence, an androgen preparation is needed that provides appropriate and constant drug delivery over long periods. To achieve this goal, a potent androgen is required that can provide effective treatment for a long period of time with the same mass of drug that is commonly used for testosterone. 7a-methyl-I 9-nortestosterone (MENT) is a synthetic androgen that is considerably more potent than testosterone (Fig. 1). A major advantage of MENT is that it is feasible to administer adequate amounts of this androgen by way of subdermal implants. Another advantage of MENT is that it does not undergo 5a-reduction to a 5a-dihydrosteroid in the prostate as does testosterone. As an element of normal physiology, the action of testosterone is amplified 3-5-fold in the prostate by its conversion to 5a-dihydrotestosterone (DHT). Since MENT avoids this amplification, a dose of this androgen sufficient to maintain normal muscle mass and gonadotrophin secretion will not overstimulate the prostate. Thus, MENT can be administered to men with the assurance that it is less likely to lead to benign prostatic hypertrophy (BPH) than is testosterone. This may be the first androgen that has this particular health benefit.
Because of the high potency of MENT and its acetate (MENTac), adequate amounts of these androgens can be delivered from implants following subdermal placement. Implants are designed to deliver doses that mimic physiological doses of testosterone on muscle and sexual performance. Several studies have shown that the biological activities of MENT and MENTac are the same in a variety of tissues, probably because MENTac is rapidly converted to MENT in vivo. The diffusion rate of MENT from several controlled-release matrices is slow relative to that of MENTac. As a consequence, there is some latitude in the choice of a matrix for implant design. Accordingly, both MENT and MENTac are being examined in several possible implants.
The present review will examine the metabolism and the biological activities of MENT. These observations form the basis of the rationale to recommend MENT as a health-promoting androgen that can be administered by an implant.
Why Is There a Need for a New Androgen?
The goal was to select a new androgen that will be an integral part of any male contraceptive method that depends on the suppression of gonadotropin secretion. Currently, LHRH vaccines as well as LHRH analogs are being investigated as pituitary blocking agents and MENT seems like a good candidate for use with both. In addition, the use of androgen as a primary method of male contraception continues to be under intense scrutiny (1). The androgens most commonly used for these purposes are the various testosterone esters. They are absorbed slowly when injected S.C. or i.m. in an oil depot. Testosterone enanthate (TE) is the most widely used replacement androgen (2, 3). While the clinical effectiveness and safety of TE are well established, it has the disadvantage of requiring i.m. or S.C. administration at 1 -3-week intervals (1, 4). Testosterone cypionate must be injected at similar intervals (5). The pharmacokinetics following the administration of these preparations show that serum testosterone reaches superphysiological levels for 2 or 3 days and then, depending on the frequency of injection, can decline to levels below normal before the next injection (6). Clearly, the need for frequent intramuscular injections and the overdose/ underdose variation is a drawback in the use of these esters. Anadur, a 19-nortestosterone ester must also be given i.m. at 1 -&week intervals at doses of 200 mg (7,8). Testosterone undecanoate, an orally active testosterone ester, is absorbed by the intestinal lymphatics; however, the drug must be taken three times daily to maintain adequate androgen support In addition, the testosterone levels achieved are variable within a subject and among different subjects (9).
Pellet implants, made of compressed testosterone crystals, are cylindrical rods for subdermal implantation (10). They are popular in Australia and the United Kingdom for the treatment of hypogonadism. The implants are inserted subdermally by a minor surgical procedure and last for 4-5 months. Pharmacokinetic studies show that serum testosterone levels reach a high concentration within 1 month and then decline steadily. Serum testosterone levels decline below the normal range before the implant completely dissolves.
To overcome the disadvantages of the highs and lows of the above parenteral preparations, NIH and WHO are investigating long-acting depot preparations. A testosterone ester (testosterone buciclate) has been shown to maintain serum testosterone levels in the normal range for up to 4 months in castrated cynomolgus monkeys after a single intramuscular injection of 40 mg of the ester (11). To achieve a similar goal in man would require the administration of approximately 1 .O g of the ester, a large dose by any measure. In another approach, testosterone is microencapsulated in a biodegradable matrix of lactide/glycolide copolymer that provides effective levels of testosterone for 2-3 months after a single intramuscular injection (1 2). The duration of action of this
In summary, all preparations that use testosterone require the administration of a large mass of the drug. In addition, esters with long side chains add additional bulk to the preparations. MENT, which is 10 times more potent than testosterone, will need to be administered in much smaller doses and thus reduce mass. The estimated daily dose of MENT is expected to be 300-500 pg. Such quantities are easily administered subdermally via sustained release preparations that can be expected to last for 1 year or longer.
In Vitro Metabolism of MENT
In the male reproductive tract and in the skin, testosterone is enzymatically converted via 5a-reductase and the 3-oxidoreductase(s) to androgens with increased activity. These metabolites of testosterone include DHT and the5a-diols. The increased activity of DHT is probably due to its increased affinity to the androgen receptor whereas the increased androgenic action of the Ba-diols is due to oxidation to DHT (1 3). Testosterone can also be aromatized to oestradiol by the enzyme aromatase which is distributed widely in many tissues. The biological role of oestradiol in the male is complex and not fully understood in men. In view of the active products that can be formed from testosterone, it was pertinent to investigate the metabolism of MENT.
5a -Reduction of MENT
The in vitro metabolism of MENT has been investigated in rat liver, ventral prostate, and epididymis (1 4). Radioactively labeled MENT was incubated with tissue homogenates. In liver homogenates three metabolites were identified: 7a-methyl-estr-4-ene-3,7-dione; 7amethyl-5~estrane-3,17/3-diol; and 7a-methyl-3-oxoestr-4-ene-l6,17@-diol. There was no evidence of 5a-dihydro products. In prostate or epididymal homogenates, there was no detectable metabolism of MENT. In parallel investigations, 48% of radiolabelled testosterone was converted to a Ba-reduced product by the prostate and epididymis. We concluded from these observations that MENT does not undergo 5a-reduction, probably because the 7a-methyl group hindered the action of the 5a-reductase. These observations lead to the postulate that compared to testosterone the relative biopotency of MENT on the prostate would be lower than that on muscle.
Aromatization of MENT
Some investigators have postulated that 19-norsteroids cannot be aromatized because of the absence of the /?-methyl group at position-19. To investigate this possibility, 3H-te~to~ter~ne or 3H-MENT were incubated with human placental microsomes in the presence of an NADPH generating system, and the phenolic metabolites were extracted. The extracted metabolites were evaluated by chromatography and by binding to estrogen receptors. These studies indicated that MENT can be metabolized to an oestrogenic compound that is most likely 7amethylestradiol. The conversion of both analogs to estrogens was blocked by an aromatase inhibitor (Table 1).
Basis for the Advantages of MENT
Following the observation that testosterone was converted to DHT in the skin and male reproductive tract, and the realization of its importance in fetal development, it was proposed that testosterone is the physiologically active steroid in many target tissues such as kidney, muscle, pituitary, and brain, since its conversion to DHT could not be demonstrated in vivo in these tissues. Thus, testosterone per se is the androgen that binds to the androgen receptors in these tissues, and the testosterone-receptor complex is the molecular entity that is localized in the nuclei of responsive cells (13). These observations alone provided reason to believe that testosterone is active in many tissues. This postulate, however, was strongly supported by the observations that 5a-reductase inhibitors do not alter the action of testosterone on such tissues (17, 18). In the male reproductive tract (excepting the testis) and sexual skin, testosterone is metabolized to DHT by 5a-reductase (19). Since DHT is 3-5 times more active than testosterone (probably because of its greater affinity for androgen receptors) (20), the action of testosterone is amplified in such tissues. This enhancement of testosterone action is believed to be necessary for the differentiation of the male reproductive tract in the fetus. This conclusion is based on studies of patients with genetically determined Sa-reductase deficiency and on the effects of 5a-reductase inhibitors on androgen-dependent differentiation (21 ).
In adult animals and humans, 5a-reductase inhibitors reduce but do not abolish the action of testosterone on the prostate and other reproductive organs since these inhibitors eliminate the amplification of but not the basal tissue response to testosterone. As a consequence, such agents have been recommended for use in men with BPH by a U.S. FDA advisory committee. Since 5areductase is also present in sexual skin, these inhibitors may also retard beard growth and reduce androgen-dependent hair loss from the scalp. Other possible biological consequences of the blockade of this enzyme in adults are not evident from studies to date but are being extensively evaluated as new inhibitors are further examined in men. Thus, there is considerable evidence to indicate that the action of testosterone is amplified in the prostate and other reproductive organs. However, at present, there is no known physiological need for amplification of the action of testosterone in adults. If this is the case then MENT should be able to provide suitable androgen replacement in hypogonadal men. The goal of treatment would be to select a dose that would maintain the metabolic and behavioral effects of testosterone without hyperstimulation of the prostate.
That there is no known physiological need for amplification of testosterone action in adults suggests that chronic use of 5a-reductase inhibitors could prevent BPH and possibly prostate cancer. Although this postulate is attractive, the potent effects of 5a-reductase inhibitors on fetal sexual differentiation and the possible transfer of these inhibitors from male to female in semen may preclude their widespread prolonged use in healthy men. Therefore, 5a-reductase inhibitors can be recommended for use in men with established prostatic hyperplasia rather than as an agent that will prevent its occurrence. Based on these considerations, we propose that an alternative approach that could be used in healthy men is to suppress testosterone secretion with an LHRH analog and then use MENT to maintain libido and the metabolic effects of testosterone. Replacement with MENT would be analogous to treatment with a 5a-reductase inhibitor since MENT cannot be reduced by 5a-reductase. If it can be demonstrated that an implant system that delivers LHRH analog plus MENT can safely be used for contraception in men then similar implants could also be used to limit the development of BPH.
We conclude that the use of MENT instead of testosterone for androgen replacement in hypogonadal men and as a component of a male contraceptive could have health-promoting effects by reducing the occurrence of prostatic disease.
7α-Methyl-19-nortestosterone (MENTR): the Population Council's contribution to research on male contraception and treatment of hypogonadism (2013)
Eberhard Nieschlaga,⁎, Narender Kumar b , Régine Sitruk-Ware
Abstract Testosterone is an essential part of all regimens for hormonal male contraception tested to date. Initial efficacy trials revealed that the half-life of the testosterone preparations available at that time was too short to be used for male contraception. The ensuing search for long-acting preparations yielded testosterone buciclate and undecanoate as well as 7α-methyl-19-nortestosterone (MENT). The following description of the principle of male hormonal contraception and the efficacy trials performed to date, the systematic development of MENT for substitution of male hypogonadism, and use in male contraception by the Population Council is reviewed here.
1. Introduction
Men are increasingly expected and willing to share the responsibility for family planning by using contraceptive methods [1]. However, traditional male methods of contraception such as periodic abstinence or coitus interruptus are associated with a relatively high rate of unwanted pregnancies as well as disturbances in sexual activity. Condoms are the oldest barrier method available, but when using condoms, conception rates remain relatively high, with 12/ 100 couples conceiving during the first year of use. Nevertheless, condom use has increased since the beginning of the AIDS epidemic, but more for protection from AIDS infection and other sexually transmitted diseases than for contraceptive purposes. Vasectomy is a safe and surgically relatively simple method for male contraception. The rate of unwanted pregnancies after vasectomy is less than 1%. The drawback of vasectomy is that it is not easily reversible. Achieving fatherhood after vasectomy requires either surgical refertilization or sperm aspiration from the epididymis or testicular sperm extraction and intracytoplasmic sperm injection into the ovum. Only about 50% of these men will ultimately become fathers.
Considering these disadvantages of the traditional male contraceptive methods mentioned above, the prerequisites for an ideal pharmacologic male contraceptive become clear, they should [2]:
• be applied independently of the sexual act,
• be acceptable for both partners,
• not interfere with libido, potency, or sexual activity,
• have neither short- nor long-term toxic side effects,
• have no impact on eventual offspring,
• be rapidly effective and fully reversible and
• be as safe and effective as comparable female methods.
Of all the different experimental approaches to pharmacological methods for male contraception tested so far, hormonal methods come closest to fulfilling the criteria set out above. The endocrine feedback mechanism operating between the hypothalamus, pituitary, and testes is the basis on which hormonal approaches to male contraception rest. Their goal is to suppress spermatogenesis and to reduce sperm concentration, if possible, to azoospermia or at least to a sperm concentration low enough to provide contraceptive protection to a degree at least as good as generally accepted female contraceptive methods.
Sperm production and secretion of testicular testosterone are so closely interwoven [3] that it has remained impossible to interrupt spermatogenesis by hormonal means without inhibiting androgen production. Inhibition of follicle-stimulating hormone (FSH) alone, e.g., by active immunization against FSH, leads to a reduction of sperm concentration but not to azoospermia, as monkey studies have shown [4]. Suppression of both FSH and luteinizing hormone (LH) will indeed lead to azoospermia, but will also induce symptoms of androgen deficiency affecting libido, erectile function, male behavior, and general metabolic processes (including erythropoiesis, protein, mineral, and bone metabolism). For this reason, inhibition of gonadotropins will always necessitate androgen administration [5]. Therefore, the principle of hormonal male contraception consists of [2]:
1. suppression of LH and FSH,
2. depletion of intratesticular testosterone and atrophy of spermatogenesis and
3. the substitution of peripheral testosterone to maintain androgenicity.
Testosterone itself is the first choice for hormonal male contraception as it simultaneously suppresses gonadotropins and maintains androgenicity, and indeed, testosterone alone was the first hormone tested for male contraception and has remained part of any steroid combination to date [5].
3. Development of MENTR for the treatment of hypogonadism
From the initial unsuccessful efficacy trial performed by the Population Council [7] and further preclinical and clinical investigations (e.g., [27]), it became clear that constant suppression of gonadotropins would be required to achieve or at least approach azoospermia in the semen of the volunteers. As the existing depot testosterone preparations at that time (i.e., testosterone enanthate and cypionate) had to be injected too frequently to be applicable in male contraception, the search for suitable depot formulation began. At that time, the Population Council had developed NorplantR as a long-acting female contraceptive based on levonorgestrel delivered from subcutaneous Silastic implants lasting for 7 years [28]. As this proved to be a very successful method for steroid delivery, the possible use of implants for testosterone delivery was obvious. However, a year's supply of testosterone for male contraception would be in the gram range and thus would have exceeded the capacity of a practical implant. Therefore, for implant delivery, a more potent androgen requiring less volume was needed. In addition, the search was made for an androgen that would not be a substrate for the 5α-reductase enzyme in order to spare the prostate from the androgenic effect. Several molecules were screened, and the final choice was MENTR.
MENTR had been synthesized by the Upjohn Company in the early 1960s as an androgenic–anabolic steroid for potential use in oncological therapy. In the immature castrated rat, MENTR had shown an apparently five times higher potency than testosterone (propionate) with regard to levator ani and seminal vesicle weights [29] and thus appeared to be an appropriate candidate for male contraception [30] as well as for androgen substitution in hypogonadal men [31]. Under C.W. Bardin's and K. Sundaram's aegis, systematic development of MENTR for clinical purposes was started. The necessary toxicology was undertaken, and a radioimmunoassay for MENTR to be used in pharmacokinetic studies in animals and humans was established [32,33]. In rats and later in humans, the high androgenic potency of MENTR could be confirmed [34]. As preclinical studies ascertained that MENTR was acceptable for human use, the manufacturing of SilasticR implants was initiated. First, implants with a length of 4.5 cm and a diameter of 2.7 cm containing 112 mg MENTR acetate were produced. When two or four of these rods were implanted subcutaneously in volunteers, MENTR serum levels ranged between 1 and 3 nmol/L, and LH and FSH were suppressed in a dose-dependent fashion during the 4-week trial period [35,36].
In an ensuing study in 16 hypogonadal men using one or two implants of slightly higher potency for 24 weeks, the suitability of MENTR for substitution purposes was demonstrated, especially in regard to sexual functions, but two special features emerged [37]. As shown earlier in monkeys [38], MENTR appeared to have a prostate-sparing effect in men since the prostate did not grow to the extent expected under full testosterone substitution. This effect was attributed to the fact that MENTR is not converted to 5αdihydrotestosterone and therefore might have less effect on prostate growth. However, in the same study, it was also observed that bone density in the hypogonadal men treated with MENTR did not reach the same level as in the control group treated with testosterone enanthate. This could indicate that the MENTR dose delivered in the study was not high enough for full androgenicity and triggered a thorough investigation into the effect of MENTR on bones. In the aged male castrated rat model, it was demonstrated that MENTR was well suited to restore fully normal bone structure if administered at the appropriate dose [39]. The supposed “tissue selectivity” of MENTR [37] in regard to prostate and bones could reflect the phenomenon of different threshold levels for the effects of testosterone (and androgens in general) for fully normal functions of tissues and organs as reflected by the occurrence of specific symptoms at specific testosterone levels when lowering testosterone levels in testosterone-treated hypogonadal men [40,41].
Overall, using the proper dose, MENTR appears to be well suited for the substitution of male hypogonadism. For this purpose, Schering Pharma further developed MENTR into a transdermal gel preparation by adding a fluor atom in position 11 (11-fluoro-7α-methyl-19-nortestosterone= eF-MENTR). In the phase, I study, effectiveness in treating sexual symptoms of hypogonadal men and reduced stimulation of the prostate could be demonstrated [42]. Despite these promising results, when Bayer acquired Schering to become Bayer HealthCare, the company decided to discontinue its research in this field. Therefore, the future of MENTR and eF-MENTR gels for the treatment of hypogonadism is uncertain at this stage.
5. Outlook
As this article shows, neither the development of MENTR in particular nor hormonal male contraception research, in general, has yet resulted in a product ready for licensing and application. However, the occasion of the 100th meeting of the Population Council's International Committee on Contraception Research provides an opportunity to pause and take stock of the 40-year history of research in hormonal male contraception.
Although the principle of hormonal male contraception has been proven, it appears to be extremely difficult to work out details of the steroid combination to be used and to bring it to the consumer. Without the input of the pharmaceutical industry, it will be impossible to complete the final steps in this development. However, the reluctance of the pharmaceutical industry to enter the field of male contraception has been additionally reinforced by the WHO decision to suspend the TU/NETE efficacy study. A concentrated effort by investigators, donor organizations, and politicians will be required to bring the industry back into the field or to take the lead in such development.
Although opinion polls among possible consumers indicate a willingness to use such methods and despite the keen interest of the media in male contraception, there is no strong urge on the part of society to develop male contraceptives. Research for female contraceptives before the arrival of the “pill” was driven by large segments of the female population fighting for gender equality and freedom from reproductive burdens. Although many men would now be willing to use a hormonal male contraceptive, there is no real force behind this intention. Men (and women) are not taking to the streets to rally for male contraception. There is a decisive gender difference between men and women in the perception of contraception. For women, contraception means personally avoiding pregnancy with all its medical, social, and economic implications, including the threat of death from childbearing. In contrast, for men, contraception is more a rational issue regarding respect for the partner and avoiding financial, social, and legal obligations of fatherhood. However, the time can be foreseen when even this rational approach may result in popular demand for male contraception, be it for the purpose of sharing responsibility for family planning by both sexes, be it for a contribution to reducing overpopulation and maintaining an ecological balance or be it for men's desire to regain reproductive power, a motive not so acceptable to advocacy groups. Until this time comes, the endurance and perseverance of organizations such as the Population Council are of utmost importance to maintain the field of male contraception research be it on an underpowered level due to lack of sufficient funding.
Wow . That's some read . I'll have a read through it all . I am due to get bloods in the next few weeks... This search for a libdio Is just not worth the way I'm feeling... Never ever felt good on trt m spent £1000`s looking for the libdio and I think it's time to stopYou need to post your most recent labs.
Weare flying blind here.
Need to know where your trough TT, FT, and estradiol sit let alone RBCs/hemoglobin/hematocrit.
Hopefully, you tested using the most accurate assays TT/estradiol (LC/MS-MS) and FT (Equilibrium Dialysis or Ultrafiltration).
You have highish SHBG so it is critical that you tested using an accurate assay.
Methandrostenolone could never replace testosterone let alone it is not something that one would use long-term due to the compound being c-17 alpha alkylated which is known to stress the liver.
The use of AAS 17α-alkylated orals such as stanozolol, oxandrolone, methyltestosterone, methandrostenolone, oxymetholone, and fluoxymesterone are notorious for driving down HDL, increasing LDL, stressing the liver and hammering down SHBG.
Even then the dose/duration of use will play a big role.
Highly doubtful you are going to run into any serious liver damage from using therapeutic does (oxandrolone/stanazolol) let alone low doses of any other c-17 alpha alkylated orals from short-term use.
No AAS would be a substitution for testosterone.
If anything there may be some merit in using 7α-methyl-19-nortestosterone (MENT) which appears to be an appropriate candidate for androgen substitution in hypogonadal men as it possesses high androgenic potency and aromatizes to 7amethylestradiol.
Mind you it is not converted to DHT let alone the studies done were on a small number of patients who were using extremely low doses (subcutaneous implants/transdermal gel) and they were not long-term (>1 yr).
Hard to say what impact this would have as a sole replacement long-term especially when it comes to libido/brain chemistry.
If you feel comfortable giving it a shot go nuts!
The main reason testosterone is used for replacement therapy over nandrolone let alone any other AAS is that testosterone drugs provide a hormone that is already produced in the body.
Let alone metabolites estradiol and DHT are needed in healthy amounts to experience the full spectrum of testosterones beneficial effects on (cardiovascular health, brain health, libido, erectile function, bone health, tendon health, immune system, lipids, and body composition).
*Natural testosterone is viewed as the best androgen for substitution in hypogonadal men. The reason behind the selection is that testosterone can be converted to DHT and E2, thus developing the full spectrum of testosterone activities in long-term substitution
*Preparations of native testosterone or its esters (aromatizable T) should be used for TTh
The history of discovery, synthesis, and development of testosterone for clinical use (2015)
Eberhard Nieschlag and Susan Nieschlag
Abstract
As the most important male hormone, testosterone has an impact on almost all organs and body functions. The biological effects of testosterone and the testes have been known since antiquity, long before testosterone was identified as an active agent. Practical applications of this knowledge were the castration of males to produce obedient servants, for punishment, for the preservation of the prepubertal soprano voice, and even for the treatment of diseases. Testes were used in organotherapy and transplanted as a treatment for symptoms of hypogonadism on a large scale, although these practices had only placebo effects. In reaction to such malpractice in the first half of the 20th-century science and the young pharmaceutical industry initiated the search for the male hormone. After several detours together with their teams in 1935, Ernst Laqueur (Amsterdam) isolated and Adolf Butenandt (Gdansk), as well as Leopold Ruzicka (Zürich), synthesized testosterone. Since then testosterone has been available for clinical use. However, when given orally, testosterone is inactivated in the liver, so parenteral forms of administration or modifications of the molecule had to be found. Over 85 years the testosterone preparations have been slowly improved so that now physiological serum levels can be achieved.
Isolation and synthesis of testosterone
The craze for such products caused concern about the image of the young field of endocrinology. The famous neurosurgeon, Harvey W Cushing (1869–1939), went so From observation the growth of a cock’s comb under the influence of transplanted testes, Moore et al. (30) in 1929 established the standardized capon comb’s test measuring androgenic activity in square centimeters of comb surface. This first bioassay facilitated the determination of androgenic activity in body products as well as in chemical solutions. In 1930 Loewe and Voss (31) used the biological effects of androgens on the accessory sex organs and developed the ‘cytological regeneration test’ which was based on the regrowth of the seminal vesicle epithelium under the influence of androgenic substances (LoeweVoss-Test). The then still hypothetical male hormone was called ‘Androkinin’. This biological test helped to resolve the question of whether only one or several androgenic steroids existed and, if more than one – which one might be the more potent.
In the dawn of testosterone emerging as a biochemical and marketable entity, and after lengthy negotiation in 1935, Ciba (Switzerland) and Schering-Kahlbaum (Germany), pharmaceutical companies active in the field, started a cooperative effort to inform each other about progress and thus forced their academic protagonists Leopold Ruzicka (1887–1976) at the Technical University of Zürich and Adolf Butenandt (1903–1995) at the then Technical University of Gdansk, to exchange their respective advances, to which the former rivals reluctantly agreed. In 1937 the Ciba-Schering cooperation was extended to include Boehringer (Germany), Chimio Roussel (France), and Organon (The Netherlands) to form a real cartel/syndicate to share knowledge, stake market claims worldwide, and agree on the pricing of the products (1, 21). While economically profitable, this syndicate is also an early example of successful academic-industrial cooperation.
In 1931 Adolf Butenandt, then at the University of Göttingen, isolated the androgenic steroid androsterone (androstan-3α-ol-17-one) from 15,000L of urine provided by young policemen from Berlin and which were processed by Schering to obtain 15mg of this substance. Butenandt considered androsterone the principal androgen (32). Ernst Laqueur (1866–1947) and his group at the University of Amsterdam and at Organon specialized in extracting hormones from animal glands. From 100kg of bull testes, they extracted and isolated 10mg of another androgen, 17β-hydroxy-4-androstene-3one, which they found to be more active than androsterone in biological tests in 1935 (33). They baptized this hormone ‘testosterone’. Although Butenandt liked neither this ‘dreadful’ name nor the competition, in the same year Butenandt and Hanisch (34) at that time at the University of Gdansk, (Fig. 2) as well as Ruzicka and Wettstein (35) in Zurich/Basel (Fig. 3), published the chemical synthesis of testosterone, thus marking the beginning of modern clinical pharmacology of testosterone and male reproductive physiology. For the synthesis of testosterone, Butenandt had started with dehydroandrosterone, while Ruzicka used a degradative approach which he also used for 17alpha-methyltestosterone, the first orally effective testosterone preparation
The close cooperation among the researchers, reinforced by the pharmaceutical companies, may explain why these discoveries were published more or less at the same time. Marius Tausk, one of the former heads of research at Organon who knew the competing protagonists personally, describes the race to testosterone isolation and synthesis very vividly and how the key respective papers were submitted for publication in a short sequence in 1935 (36).
In 1939 Butenandt and Ruzicka received the Nobel Prize for chemistry jointly, Butenandt ‘for his work on sex hormones (estrogen, progesterone, and androsterone – but not for testosterone!) and Ruzicka for his work on polymethylenes and higher terpenes and also not explicitly for testosterone!
Nevertheless, neither laureate could attend the prize ceremony in Stockholm. Butenandt had become director of the Institute for Biochemistry of the KaiserWilhelm-Society in Berlin in 1936; he was prevented by the Nazi regime from accepting the prize since Hitler had forbidden Germans to accept the Nobel Prize after, in 1937, the Nobel Prize for Peace had been awarded to Carl von Ossietzky, a journalist and strong opponent of the regime. In 1949, at the Swedish Consulate in Frankfurt, Butenandt received the Nobel Prize diploma and the medal, but not the money, since according to the statutes, the prize money must be collected within a year.
Incidentally, in 1939 the same indignity was suffered by the Laureate for the Nobel Prize for Medicine, Gerhard Domagk (1894–1964) who worked at the Bayer Company and was honored for his invention of the first clinically used sulfonamide Prontosil®. Domagk was even imprisoned for a few days for accepting the honor and only in 1947 received the Nobel Prize documents from the Swedish King in Stockholm, but – for the same reason as Butenandt – no money. (By the way, Domagk started his academic career between 1925 and 1929 at the University Hospitals in Münster and therefore the author’s institutional street address is named after him.) (37). Back to Butenandt, it should be noted that after the war, his research concentrated on insect hormones and he became president of the Max-Planck-Society (the former Kaiser-Wilhelm-Society), serving from 1960 to 1972.
As Ruzicka was also not able to travel to Stockholm because of turmoil caused by the beginning of World War II, on January 16, 1940 – well within a year – at a special ceremony in Zűrich, the prize was handed over to Ruzicka by the Swedish ambassador in Switzerland, Baron H G Beck-Friis (Fig. 4). After the war had ended, Ruzicka delivered his Nobel Prize lecture on December 12, 1945. In this lecture he explained how research on ‘multimembered rings and higher terpenes guided him to steroids and to testosterone as ‘cholesterol could be regarded as a triterpenoid’ (38). In the 1920s he worked in the perfume industry in Geneva (Switzerland) and Holzminden (Germany) to elucidate the chemical formulas and synthesis of fragrances. His major achievement was the structural analysis and synthesis of the polycyclical ketones such as muscone, the scent in musk pods (preputial glands of the musk deer), civetone from civetts, and santanol from sandalwood, important ingredients in perfumes which before chemical synthesis had to be extracted from their natural sources. In 1929 he became a professor of organic chemistry at the ETH in Zűrich and teamed up with researchers at Ciba in Basel. Ciba was interested in his knowledge of cyclical structures and cooperated with him in the field of triterpenes and steroids, another class of cyclical substances. For the synthesis of testosterone Ruzicka started from cholesterol and used the same degradative approach as for the synthesis of fragrances.
As Ruzicka remarked in autobiographical notes, beyond scientific recognition his research work was also financially rewarding: ‘The patents for the degradative synthesis of testosterone and methyltestosterone earned me during subsequent years an enormous (compared with my professorial standard) amount of money as royalties from Ciba in Basel and Ciba in the USA’. (39). In the year 1939 alone Ciba transferred 56,744 Swiss Francs to Ruzicka as royalties (21). Part of this money was invested in a collection of 17th-century Flemish and Dutch paintings which Ruzicka donated to the Kunsthalle Zürich in 1947 (39) where they form a substantial part of the museum’s inventory
Why Laqueur’s identification of testosterone rather than androsterone as the most important male sex hormone was not recognized by the Nobel Committee in 1939 remains unclear. Laqueur was born in 1880 and grew up near Breslau (Silesia), at that time still in Germany, and received his medical education and degrees in Germany. In 1920 he became a professor of pharmacology at the University of Amsterdam. In 1923 he co-founded Organon located next to the slaughterhouses in Oss (The Netherlands) to extract insulin from pig pancreas. Organon became the first European producer of insulin for the treatment of diabetes. In 1930 Laqueur acquired Dutch nationality. When the Germans invaded The Netherlands in 1940, Laqueur lost his position because of his Jewish background and had to surrender his shares in Organon, but was not further persecuted in contrast to some members of his family.
New syndromes of hypogonadism
It may not have been a coincidence, but a sign of heightened interest in the clinics of hypogonadism that at the same period when testosterone became available for clinical use, that is, when rational treatment became possible, major syndromes of primary and secondary hypogonadism were first described, that is the Klinefelter syndrome in 1942 (40) and the Kallmann syndrome in 1944 (41). Pasqualini and Bur (42) described the fertile eunuch syndrome, characterized by all symptoms of lack of testosterone, but with active spermatogenesis. Also at that time, the symptoms of the aging male were first described systematically, but unfortunately incorrectly termed as ‘male climacteric’ (43), starting a controversial discussion that continues until today. Del Castillo et al. (44) published in1947 the first five cases suffering from Sertoli-cell-only syndrome. Reifenstein (45) first described a syndrome with partial androgen insensitivity (PAIS) that carries his name to date and Morris (46) published the first cases of complete androgen insensitivity (CAIS) as ‘testicular feminization in male pseudohermaphroditism – of course without knowing anything about the androgen receptor or androgen receptor mutations.
Early warning for testosterone
Around the same time, Huggins also posted his warning about testosterone influencing prostate carcinoma (47), which prevailed until quite recently and led to castration as the major treatment of prostate carcinoma, when androgen deprivation therapy (ADT) by GnRH analogs or antiandrogens was introduced instead. Huggins’ statement ‘Cancer of the prostate is activated by androgen injections’ induced a general fear of testosterone, especially among urologists, which prevented testosterone treatment in many patients who might have needed it. Only recently it became clear that neither endogenous serum testosterone levels (48) nor testosterone treatment (49) have an impact on prostate carcinogenesis. Nowadays under careful supervision testosterone treatment is even considered for patients suffering from testosterone deficiency after radical prostatectomy and castration (50).
Development of testosterone preparations for clinical use (1)
Soon after its synthesis, it became clear that, in reasonable doses, testosterone was not effective orally or – as we know it today – would require extremely high doses which were simply not available and/or too expensive. Today we know that the lack of oral effectiveness is due to the inactivation of testosterone by the first-pass effects in the liver. Three approaches were used to overcome this problem:
1. Chemical modification of the steroid molecule,
2. parenteral application and
3. esterification in position 17β of the testosterone molecule.
For a more complete description of the many testosterone preparations and routes of administration, the reader is referred to a review by Behre and Nieschlag (51). A major goal of the efforts to produce new testosterone preparations for clinical use was to optimize the treatment of hypogonadism. Later, when serum levels of testosterone could be determined, an additional goal was to mimic physiological serum testosterone levels as closely as possible (52). As shown in the ensuing text, it took quite a long to reach these goals.
As mentioned above, in 1935 together with testosterone Ruzicka et al. (53) synthesized 17α-methyl-testosterone and demonstrated its oral effectiveness. Since the 17α-configuration protected against degradation in the liver, it soon was well accepted for clinical use (54). However, due to its 17α-structure it was liver toxic, especially under long-term use or at higher doses (55), a feature shared by all 17α substituted androgens. In error some physicians considered liver toxicity a general feature of testosterone preparations, thus making testosterone a dangerous drug. Eventually, at least in Europe, 17α-methyl-testosterone became obsolete for clinical use after the introduction of orally effective testosterone undecanoate in the late 1970s (see below).
As native testosterone proved to be ineffective orally, parenteral routes were explored. Subdermal testosterone pellet implants were the first to be investigated (56) and pellets are still in use today. Their application requires a small operation and harbors the risk of infection and extrusion. However, if enough pellets are implanted, they may provide a substitution for up to half a year and are sporadically still used today (51).
When injected, testosterone has an extremely short half-life of only 10min and as such is not suited for substitution purposes. Therefore, the third possibility of making testosterone clinically effective is esterification at the 17β-hydroxy group of the molecule, making it suitable for intramuscular injection. Testosterone propionate was the first of these esters marketed by Ciba and by Schering in 1936. However, this ester has a short half-life so effective serum levels are reached for only 1–2 days.
Following the propionate ester, testosterone enanthate was synthesized by Junkmann (57) at Schering and marketed as intramuscular Testoviron® Depot injection in 250mg doses, providing substitution for 2–3 weeks (58). However, the pharmacokinetics are characterized by transient supraphysiological peaks for a few days, followed by a slow decline to levels below the lower limit of normal. Although patients do not appreciate these uneven swings in mood, activity, and libido between injections, this remained the major testosterone preparation for the substitution of hypogonadism for half a century and is still used today as a cost-effective alternative to more modern preparations.
Other parenteral routes were tested in the course of the steroid’s history during which testosterone suppositories were marketed by Ferring (59), but yielded rather unpredictable serum levels (58) and are no longer commercially available. A more recent development in this area is bioadhesive buccal testosterone tablets, placed on the gingiva and resulting in effective serum levels if applied twice daily (60). However, due to low patient compliance, they have never penetrated the market. The nasal route has also been explored (61) and has recently been revived for treatment of hypogonadism (62)
From the 1950s to the 1970s, the pharmaceutical industry tried to modify the chemical structure of the molecule in order to disentangle the various effects and produce predominantly erythropoietic, osteogenic, or anabolic steroids. Although more than a thousand of these androgens were synthesized (63), it proved impossible to produce androgens with only one desired effect out of the wide spectrum of testosterone activities. Nevertheless, while some anabolic androgenic steroids (AASs) were clinically used, they disappeared again in the wake of evidence-based medicine. However, they retained a shadow existence for doping in sports and bodybuilding, potentially causing considerable undesired effects (64)
In the 1970s the orally effective testosterone undecanoate, absorbed from the gut via the lymph to avoid the first-pass effect in the liver (65) had been added to the spectrum of testosterone preparations available for replacement therapy. Initial clinical testing revealed that oral testosterone undecanoate was best absorbed with a meal, but the testosterone peaks were short-lived so 3–4 capsules had to be taken during the day in order to produce effective serum levels (66). Oral testosterone undecanoate was introduced to the market worldwide in the late 1970s – except in the USA – and is still in wide use despite rather variable serum testosterone profiles.
In the 1970s the WHO Human Reproduction Program as well as the Population Council of the Rockefeller Foundation had identified male contraception as an unmet need for family planning and as a means against global overpopulation.
Hormonal male contraception based on the combination of testosterone and progestin was at that time – and remains so to date – the most likely candidate for general use. However, the existing testosterone preparations required too frequent applications (for review of clinical trials see (67)). To overcome this deficiency both organizations started programs in search of long-acting testosterone preparations. Under the auspices of WHO, testosterone buciclate was synthesized (68) and identified as a long-acting preparation, well suited for male contraception – and by the same token, also for substitution (69). However, no pharmaceutical company could be persuaded to develop this promising preparation further (70), so in its ensuing clinical trials for male contraception, WHO switched to intramuscular testosterone undecanoate as described below and is now widely used for the treatment of hypogonadism.
Meanwhile, the Population Council had turned to 7α-methyl-19-nortestosterone (MENT) as its preferred androgen for male contraception. This androgen might have the advantage of lacking conversion to DHT and thereby have little effect on the prostate. As MENT has a rather short half-life, it was administered via subdermal Silastic implants, delivering the active substance for a year – or perhaps even longer – thus being well suited for contraception as well as for substitution (71, 72). However, the company interested in further clinical research with this androgen dropped its plans in the wake of being taken over by another company not interested in the male.
In the mid-1990s, transdermal testosterone films applied to the scrotal skin became the first transdermal testosterone preparation in clinical use. Invented by Virgil Place (1924–2012) at ALZA in Palo Alto (CA) and first tested in clinical trials in Münster (73, 74), they showed excellent pharmacokinetic and clinical results and, for the first time, physiological testosterone serum levels could be achieved. Patients were very satisfied with this physiological pharmacokinetic profile, as long-term substitution revealed. However, physicians were reluctant to prescribe a medication to be applied to the scrotum, preferring a subsequently developed non-scrotal testosterone system (75). This, however, caused unpleasant skin reactions as it required an alcoholic enhancer to drive testosterone through the skin (1).
For this reason, the advent of transdermal testosterone gels in 2000 was welcomed for substitution (76). These testosterone-containing gels are applied to the upper arms, shoulders, or abdomen. Those applied in the morning result in physiological serum testosterone levels, almost mimicking the normal diurnal rhythm. Precautions against interpersonal transfer have to be taken, mostly by covering the application sites with a T-shirt. Of the various gels available today, the one with a high 2.5% testosterone concentration can be washed off the skin shortly after application, thereby reducing the danger of contaminating children or women. It has also been tested for scrotal application. Because of the high absorptive capacity of the scrotal skin, only 20% of the gel needed for the non-scrotal application is required, making this form of application economically and ecologically desirable (77), but has not yet been licensed for that purpose.
Finally, in 2004, the intramuscular testosterone undecanoate preparation entered the market and soon achieved great popularity as a real testosterone depot preparation. Testosterone undecanoate, originally provided in oral capsules (see above), had been turned into an injectable preparation by Chinese investigators using tea seed oil as a vehicle. When the author came across it at a meeting in Bejing in 1993 (78), samples were brought to Germany, injected into monkeys, and showed a surprisingly long half-life (79), which could be confirmed in volunteering hypogonadal men who all showed serum levels in the normal range for several weeks (80). When finally a company could be interested in this fascinating preparation, tea seed oil was replaced by castor oil as a vehicle and the injection intervals could be extended to 12 weeks of physiological serum testosterone levels (81, 82). Since 2004, this preparation available in 1000mg ampoules has been licensed in over 100 countries. The latest approval was issued by the FDA in 2014 – however in 750mg doses.
Outlook
Although the effects of testosterone were known for ages, the actual molecule itself was isolated and synthesized only within the last eight decades, that is, in 1935. Since then testosterone has been in clinical use for the substitution of hypogonadal patients. Substitution modalities have been improved slowly by the production of testosterone preparations resulting in physiological serum levels as requested (52). The most recent developments, transdermal testosterone gels, and intramuscular testosterone undecanoate are close to this goal but have not yet reached perfection. Clinical trials for selective androgen receptor modulators (SARMs) have started, but as their goal is selected, testosterone actions such as those required for treatment of sarcopenia or osteoporosis, will not be suited for substitution of hypogonadism, where the full spectrum of testosterone actions is required (83). So far, they seem to be suffering the same fate as androgenic anabolic steroids, even before they have been licensed for clinical use by the drug authorities. As unlicensed substances, they are applied as performance-enhancing substances and for doping. Ultimately, for ideal substitution hope rests on human stem Leydig cells transplanted to hypogonadal patients (84). The goal for these patients – at least those with an intact hypothalamic-pituitary system – would be that the testosterone production required would be provided by the transplanted Leydig cells and would be self-regulated by feedback to LH. These patients would then become independent of exogenous testosterone preparations.
Keep in mind this paper is from 1993and we have come a long way regarding testosterone/DHT and the prostate.
7a-Methyl-Nortestosterone (MENT): The Optimal Androgen For Male Contraception (1993)
Kalyan Sundaram, Narender Kumar and C. Wayne Bardin
Many methods of contraception involve the use of drugs that affect the secretion of hormones essential for reproduction. Oestrogens and progestins have been used for contraception in women as inhibitors of gonadotrophin secretion and ovulation. Similarly, androgens must be used in methods of fertility control for men that block gonadotrophin secretion. Androgen supplementation currently involves large, frequent doses of testosterone esters that are associated with wide fluctuations of plasma testosterone levels. Hence, there Is a need for an androgen preparation that provides appropriate, continuous replacement doses over long periods. To achieve this goal, 7 a-methyl-19. nortestosterone (MENT), a synthetic androgen that Is considerably more potent than testosterone, is suitable. As a consequence, it is feasible to administer this androgen as a substitute for testosterone for 1 year by subdermal implants. Another important feature of MENT is that it does not undergo Sa- reduction In the prostate as does testosterone. As a consequence, a dose of MENT sufficient to maintain normal muscle mass and gonadotrophin secretion will not hyperstimulate the prostate because its action in this organ is not amplified 88 Is that of testosterone. Thus, MENT can be administered to men with the assurance that It will be less prone to cause damage to the prostate than testosterone.
Conclusions: (I) MENT is the first androgen that has a health benefit compared to testosterone; (11) MENT will be promoted as one component of a two-implant system for male contraception, the other component is an implant that All releases an LHRH analog; (lii) MENT has potential uses In patients with a variety of disorders, including hypogonadism, prostatic hyperplasia, and muscle wasting.
Introduction
Some methods of contraception involve the use of drugs that affect the secretion of hormones essential for reproduction. Combined oral contraceptives are used as inhibitors of pituitary gonadotrophins secretion, ovarian hormone secretion, and ovulation. The estrogens and progestins in these contraceptives effectively replace the steroid output of the ovaries that they so efficiently reduce. Methods of fertility control in men that block gonadotrophin secretion and sperm production will also decrease testosterone production. Therefore, androgens will be an essential part of such methods. The most common androgen supplementation involves the administration of large doses of testosterone esters that require frequent injections and that are, in turn, associated with wide fluctuations of plasma testosterone levels. Hence, an androgen preparation is needed that provides appropriate and constant drug delivery over long periods. To achieve this goal, a potent androgen is required that can provide effective treatment for a long period of time with the same mass of drug that is commonly used for testosterone. 7a-methyl-I 9-nortestosterone (MENT) is a synthetic androgen that is considerably more potent than testosterone (Fig. 1). A major advantage of MENT is that it is feasible to administer adequate amounts of this androgen by way of subdermal implants. Another advantage of MENT is that it does not undergo 5a-reduction to a 5a-dihydrosteroid in the prostate as does testosterone. As an element of normal physiology, the action of testosterone is amplified 3-5-fold in the prostate by its conversion to 5a-dihydrotestosterone (DHT). Since MENT avoids this amplification, a dose of this androgen sufficient to maintain normal muscle mass and gonadotrophin secretion will not overstimulate the prostate. Thus, MENT can be administered to men with the assurance that it is less likely to lead to benign prostatic hypertrophy (BPH) than is testosterone. This may be the first androgen that has this particular health benefit.
Because of the high potency of MENT and its acetate (MENTac), adequate amounts of these androgens can be delivered from implants following subdermal placement. Implants are designed to deliver doses that mimic physiological doses of testosterone on muscle and sexual performance. Several studies have shown that the biological activities of MENT and MENTac are the same in a variety of tissues, probably because MENTac is rapidly converted to MENT in vivo. The diffusion rate of MENT from several controlled-release matrices is slow relative to that of MENTac. As a consequence, there is some latitude in the choice of a matrix for implant design. Accordingly, both MENT and MENTac are being examined in several possible implants.
The present review will examine the metabolism and the biological activities of MENT. These observations form the basis of the rationale to recommend MENT as a health-promoting androgen that can be administered by an implant.
Why Is There a Need for a New Androgen?
The goal was to select a new androgen that will be an integral part of any male contraceptive method that depends on the suppression of gonadotropin secretion. Currently, LHRH vaccines as well as LHRH analogs are being investigated as pituitary blocking agents and MENT seems like a good candidate for use with both. In addition, the use of androgen as a primary method of male contraception continues to be under intense scrutiny (1). The androgens most commonly used for these purposes are the various testosterone esters. They are absorbed slowly when injected S.C. or i.m. in an oil depot. Testosterone enanthate (TE) is the most widely used replacement androgen (2, 3). While the clinical effectiveness and safety of TE are well established, it has the disadvantage of requiring i.m. or S.C. administration at 1 -3-week intervals (1, 4). Testosterone cypionate must be injected at similar intervals (5). The pharmacokinetics following the administration of these preparations show that serum testosterone reaches superphysiological levels for 2 or 3 days and then, depending on the frequency of injection, can decline to levels below normal before the next injection (6). Clearly, the need for frequent intramuscular injections and the overdose/ underdose variation is a drawback in the use of these esters. Anadur, a 19-nortestosterone ester must also be given i.m. at 1 -&week intervals at doses of 200 mg (7,8). Testosterone undecanoate, an orally active testosterone ester, is absorbed by the intestinal lymphatics; however, the drug must be taken three times daily to maintain adequate androgen support In addition, the testosterone levels achieved are variable within a subject and among different subjects (9).
Pellet implants, made of compressed testosterone crystals, are cylindrical rods for subdermal implantation (10). They are popular in Australia and the United Kingdom for the treatment of hypogonadism. The implants are inserted subdermally by a minor surgical procedure and last for 4-5 months. Pharmacokinetic studies show that serum testosterone levels reach a high concentration within 1 month and then decline steadily. Serum testosterone levels decline below the normal range before the implant completely dissolves.
To overcome the disadvantages of the highs and lows of the above parenteral preparations, NIH and WHO are investigating long-acting depot preparations. A testosterone ester (testosterone buciclate) has been shown to maintain serum testosterone levels in the normal range for up to 4 months in castrated cynomolgus monkeys after a single intramuscular injection of 40 mg of the ester (11). To achieve a similar goal in man would require the administration of approximately 1 .O g of the ester, a large dose by any measure. In another approach, testosterone is microencapsulated in a biodegradable matrix of lactide/glycolide copolymer that provides effective levels of testosterone for 2-3 months after a single intramuscular injection (1 2). The duration of action of this
In summary, all preparations that use testosterone require the administration of a large mass of the drug. In addition, esters with long side chains add additional bulk to the preparations. MENT, which is 10 times more potent than testosterone, will need to be administered in much smaller doses and thus reduce mass. The estimated daily dose of MENT is expected to be 300-500 pg. Such quantities are easily administered subdermally via sustained release preparations that can be expected to last for 1 year or longer.
In Vitro Metabolism of MENT
In the male reproductive tract and in the skin, testosterone is enzymatically converted via 5a-reductase and the 3-oxidoreductase(s) to androgens with increased activity. These metabolites of testosterone include DHT and the5a-diols. The increased activity of DHT is probably due to its increased affinity to the androgen receptor whereas the increased androgenic action of the Ba-diols is due to oxidation to DHT (1 3). Testosterone can also be aromatized to oestradiol by the enzyme aromatase which is distributed widely in many tissues. The biological role of oestradiol in the male is complex and not fully understood in men. In view of the active products that can be formed from testosterone, it was pertinent to investigate the metabolism of MENT.
5a -Reduction of MENT
The in vitro metabolism of MENT has been investigated in rat liver, ventral prostate, and epididymis (1 4). Radioactively labeled MENT was incubated with tissue homogenates. In liver homogenates three metabolites were identified: 7a-methyl-estr-4-ene-3,7-dione; 7amethyl-5~estrane-3,17/3-diol; and 7a-methyl-3-oxoestr-4-ene-l6,17@-diol. There was no evidence of 5a-dihydro products. In prostate or epididymal homogenates, there was no detectable metabolism of MENT. In parallel investigations, 48% of radiolabelled testosterone was converted to a Ba-reduced product by the prostate and epididymis. We concluded from these observations that MENT does not undergo 5a-reduction, probably because the 7a-methyl group hindered the action of the 5a-reductase. These observations lead to the postulate that compared to testosterone the relative biopotency of MENT on the prostate would be lower than that on muscle.
Aromatization of MENT
Some investigators have postulated that 19-norsteroids cannot be aromatized because of the absence of the /?-methyl group at position-19. To investigate this possibility, 3H-te~to~ter~ne or 3H-MENT were incubated with human placental microsomes in the presence of an NADPH generating system, and the phenolic metabolites were extracted. The extracted metabolites were evaluated by chromatography and by binding to estrogen receptors. These studies indicated that MENT can be metabolized to an oestrogenic compound that is most likely 7amethylestradiol. The conversion of both analogs to estrogens was blocked by an aromatase inhibitor (Table 1).
Basis for the Advantages of MENT
Following the observation that testosterone was converted to DHT in the skin and male reproductive tract, and the realization of its importance in fetal development, it was proposed that testosterone is the physiologically active steroid in many target tissues such as kidney, muscle, pituitary, and brain, since its conversion to DHT could not be demonstrated in vivo in these tissues. Thus, testosterone per se is the androgen that binds to the androgen receptors in these tissues, and the testosterone-receptor complex is the molecular entity that is localized in the nuclei of responsive cells (13). These observations alone provided reason to believe that testosterone is active in many tissues. This postulate, however, was strongly supported by the observations that 5a-reductase inhibitors do not alter the action of testosterone on such tissues (17, 18). In the male reproductive tract (excepting the testis) and sexual skin, testosterone is metabolized to DHT by 5a-reductase (19). Since DHT is 3-5 times more active than testosterone (probably because of its greater affinity for androgen receptors) (20), the action of testosterone is amplified in such tissues. This enhancement of testosterone action is believed to be necessary for the differentiation of the male reproductive tract in the fetus. This conclusion is based on studies of patients with genetically determined Sa-reductase deficiency and on the effects of 5a-reductase inhibitors on androgen-dependent differentiation (21 ).
In adult animals and humans, 5a-reductase inhibitors reduce but do not abolish the action of testosterone on the prostate and other reproductive organs since these inhibitors eliminate the amplification of but not the basal tissue response to testosterone. As a consequence, such agents have been recommended for use in men with BPH by a U.S. FDA advisory committee. Since 5areductase is also present in sexual skin, these inhibitors may also retard beard growth and reduce androgen-dependent hair loss from the scalp. Other possible biological consequences of the blockade of this enzyme in adults are not evident from studies to date but are being extensively evaluated as new inhibitors are further examined in men. Thus, there is considerable evidence to indicate that the action of testosterone is amplified in the prostate and other reproductive organs. However, at present, there is no known physiological need for amplification of the action of testosterone in adults. If this is the case then MENT should be able to provide suitable androgen replacement in hypogonadal men. The goal of treatment would be to select a dose that would maintain the metabolic and behavioral effects of testosterone without hyperstimulation of the prostate.
That there is no known physiological need for amplification of testosterone action in adults suggests that chronic use of 5a-reductase inhibitors could prevent BPH and possibly prostate cancer. Although this postulate is attractive, the potent effects of 5a-reductase inhibitors on fetal sexual differentiation and the possible transfer of these inhibitors from male to female in semen may preclude their widespread prolonged use in healthy men. Therefore, 5a-reductase inhibitors can be recommended for use in men with established prostatic hyperplasia rather than as an agent that will prevent its occurrence. Based on these considerations, we propose that an alternative approach that could be used in healthy men is to suppress testosterone secretion with an LHRH analog and then use MENT to maintain libido and the metabolic effects of testosterone. Replacement with MENT would be analogous to treatment with a 5a-reductase inhibitor since MENT cannot be reduced by 5a-reductase. If it can be demonstrated that an implant system that delivers LHRH analog plus MENT can safely be used for contraception in men then similar implants could also be used to limit the development of BPH.
We conclude that the use of MENT instead of testosterone for androgen replacement in hypogonadal men and as a component of a male contraceptive could have health-promoting effects by reducing the occurrence of prostatic disease.
7α-Methyl-19-nortestosterone (MENTR): the Population Council's contribution to research on male contraception and treatment of hypogonadism (2013)
Eberhard Nieschlaga,⁎, Narender Kumar b , Régine Sitruk-Ware
Abstract Testosterone is an essential part of all regimens for hormonal male contraception tested to date. Initial efficacy trials revealed that the half-life of the testosterone preparations available at that time was too short to be used for male contraception. The ensuing search for long-acting preparations yielded testosterone buciclate and undecanoate as well as 7α-methyl-19-nortestosterone (MENT). The following description of the principle of male hormonal contraception and the efficacy trials performed to date, the systematic development of MENT for substitution of male hypogonadism, and use in male contraception by the Population Council is reviewed here.
1. Introduction
Men are increasingly expected and willing to share the responsibility for family planning by using contraceptive methods [1]. However, traditional male methods of contraception such as periodic abstinence or coitus interruptus are associated with a relatively high rate of unwanted pregnancies as well as disturbances in sexual activity. Condoms are the oldest barrier method available, but when using condoms, conception rates remain relatively high, with 12/ 100 couples conceiving during the first year of use. Nevertheless, condom use has increased since the beginning of the AIDS epidemic, but more for protection from AIDS infection and other sexually transmitted diseases than for contraceptive purposes. Vasectomy is a safe and surgically relatively simple method for male contraception. The rate of unwanted pregnancies after vasectomy is less than 1%. The drawback of vasectomy is that it is not easily reversible. Achieving fatherhood after vasectomy requires either surgical refertilization or sperm aspiration from the epididymis or testicular sperm extraction and intracytoplasmic sperm injection into the ovum. Only about 50% of these men will ultimately become fathers.
Considering these disadvantages of the traditional male contraceptive methods mentioned above, the prerequisites for an ideal pharmacologic male contraceptive become clear, they should [2]:
• be applied independently of the sexual act,
• be acceptable for both partners,
• not interfere with libido, potency, or sexual activity,
• have neither short- nor long-term toxic side effects,
• have no impact on eventual offspring,
• be rapidly effective and fully reversible and
• be as safe and effective as comparable female methods.
Of all the different experimental approaches to pharmacological methods for male contraception tested so far, hormonal methods come closest to fulfilling the criteria set out above. The endocrine feedback mechanism operating between the hypothalamus, pituitary, and testes is the basis on which hormonal approaches to male contraception rest. Their goal is to suppress spermatogenesis and to reduce sperm concentration, if possible, to azoospermia or at least to a sperm concentration low enough to provide contraceptive protection to a degree at least as good as generally accepted female contraceptive methods.
Sperm production and secretion of testicular testosterone are so closely interwoven [3] that it has remained impossible to interrupt spermatogenesis by hormonal means without inhibiting androgen production. Inhibition of follicle-stimulating hormone (FSH) alone, e.g., by active immunization against FSH, leads to a reduction of sperm concentration but not to azoospermia, as monkey studies have shown [4]. Suppression of both FSH and luteinizing hormone (LH) will indeed lead to azoospermia, but will also induce symptoms of androgen deficiency affecting libido, erectile function, male behavior, and general metabolic processes (including erythropoiesis, protein, mineral, and bone metabolism). For this reason, inhibition of gonadotropins will always necessitate androgen administration [5]. Therefore, the principle of hormonal male contraception consists of [2]:
1. suppression of LH and FSH,
2. depletion of intratesticular testosterone and atrophy of spermatogenesis and
3. the substitution of peripheral testosterone to maintain androgenicity.
Testosterone itself is the first choice for hormonal male contraception as it simultaneously suppresses gonadotropins and maintains androgenicity, and indeed, testosterone alone was the first hormone tested for male contraception and has remained part of any steroid combination to date [5].
3. Development of MENTR for the treatment of hypogonadism
From the initial unsuccessful efficacy trial performed by the Population Council [7] and further preclinical and clinical investigations (e.g., [27]), it became clear that constant suppression of gonadotropins would be required to achieve or at least approach azoospermia in the semen of the volunteers. As the existing depot testosterone preparations at that time (i.e., testosterone enanthate and cypionate) had to be injected too frequently to be applicable in male contraception, the search for suitable depot formulation began. At that time, the Population Council had developed NorplantR as a long-acting female contraceptive based on levonorgestrel delivered from subcutaneous Silastic implants lasting for 7 years [28]. As this proved to be a very successful method for steroid delivery, the possible use of implants for testosterone delivery was obvious. However, a year's supply of testosterone for male contraception would be in the gram range and thus would have exceeded the capacity of a practical implant. Therefore, for implant delivery, a more potent androgen requiring less volume was needed. In addition, the search was made for an androgen that would not be a substrate for the 5α-reductase enzyme in order to spare the prostate from the androgenic effect. Several molecules were screened, and the final choice was MENTR.
MENTR had been synthesized by the Upjohn Company in the early 1960s as an androgenic–anabolic steroid for potential use in oncological therapy. In the immature castrated rat, MENTR had shown an apparently five times higher potency than testosterone (propionate) with regard to levator ani and seminal vesicle weights [29] and thus appeared to be an appropriate candidate for male contraception [30] as well as for androgen substitution in hypogonadal men [31]. Under C.W. Bardin's and K. Sundaram's aegis, systematic development of MENTR for clinical purposes was started. The necessary toxicology was undertaken, and a radioimmunoassay for MENTR to be used in pharmacokinetic studies in animals and humans was established [32,33]. In rats and later in humans, the high androgenic potency of MENTR could be confirmed [34]. As preclinical studies ascertained that MENTR was acceptable for human use, the manufacturing of SilasticR implants was initiated. First, implants with a length of 4.5 cm and a diameter of 2.7 cm containing 112 mg MENTR acetate were produced. When two or four of these rods were implanted subcutaneously in volunteers, MENTR serum levels ranged between 1 and 3 nmol/L, and LH and FSH were suppressed in a dose-dependent fashion during the 4-week trial period [35,36].
In an ensuing study in 16 hypogonadal men using one or two implants of slightly higher potency for 24 weeks, the suitability of MENTR for substitution purposes was demonstrated, especially in regard to sexual functions, but two special features emerged [37]. As shown earlier in monkeys [38], MENTR appeared to have a prostate-sparing effect in men since the prostate did not grow to the extent expected under full testosterone substitution. This effect was attributed to the fact that MENTR is not converted to 5αdihydrotestosterone and therefore might have less effect on prostate growth. However, in the same study, it was also observed that bone density in the hypogonadal men treated with MENTR did not reach the same level as in the control group treated with testosterone enanthate. This could indicate that the MENTR dose delivered in the study was not high enough for full androgenicity and triggered a thorough investigation into the effect of MENTR on bones. In the aged male castrated rat model, it was demonstrated that MENTR was well suited to restore fully normal bone structure if administered at the appropriate dose [39]. The supposed “tissue selectivity” of MENTR [37] in regard to prostate and bones could reflect the phenomenon of different threshold levels for the effects of testosterone (and androgens in general) for fully normal functions of tissues and organs as reflected by the occurrence of specific symptoms at specific testosterone levels when lowering testosterone levels in testosterone-treated hypogonadal men [40,41].
Overall, using the proper dose, MENTR appears to be well suited for the substitution of male hypogonadism. For this purpose, Schering Pharma further developed MENTR into a transdermal gel preparation by adding a fluor atom in position 11 (11-fluoro-7α-methyl-19-nortestosterone= eF-MENTR). In the phase, I study, effectiveness in treating sexual symptoms of hypogonadal men and reduced stimulation of the prostate could be demonstrated [42]. Despite these promising results, when Bayer acquired Schering to become Bayer HealthCare, the company decided to discontinue its research in this field. Therefore, the future of MENTR and eF-MENTR gels for the treatment of hypogonadism is uncertain at this stage.
5. Outlook
As this article shows, neither the development of MENTR in particular nor hormonal male contraception research, in general, has yet resulted in a product ready for licensing and application. However, the occasion of the 100th meeting of the Population Council's International Committee on Contraception Research provides an opportunity to pause and take stock of the 40-year history of research in hormonal male contraception.
Although the principle of hormonal male contraception has been proven, it appears to be extremely difficult to work out details of the steroid combination to be used and to bring it to the consumer. Without the input of the pharmaceutical industry, it will be impossible to complete the final steps in this development. However, the reluctance of the pharmaceutical industry to enter the field of male contraception has been additionally reinforced by the WHO decision to suspend the TU/NETE efficacy study. A concentrated effort by investigators, donor organizations, and politicians will be required to bring the industry back into the field or to take the lead in such development.
Although opinion polls among possible consumers indicate a willingness to use such methods and despite the keen interest of the media in male contraception, there is no strong urge on the part of society to develop male contraceptives. Research for female contraceptives before the arrival of the “pill” was driven by large segments of the female population fighting for gender equality and freedom from reproductive burdens. Although many men would now be willing to use a hormonal male contraceptive, there is no real force behind this intention. Men (and women) are not taking to the streets to rally for male contraception. There is a decisive gender difference between men and women in the perception of contraception. For women, contraception means personally avoiding pregnancy with all its medical, social, and economic implications, including the threat of death from childbearing. In contrast, for men, contraception is more a rational issue regarding respect for the partner and avoiding financial, social, and legal obligations of fatherhood. However, the time can be foreseen when even this rational approach may result in popular demand for male contraception, be it for the purpose of sharing responsibility for family planning by both sexes, be it for a contribution to reducing overpopulation and maintaining an ecological balance or be it for men's desire to regain reproductive power, a motive not so acceptable to advocacy groups. Until this time comes, the endurance and perseverance of organizations such as the Population Council are of utmost importance to maintain the field of male contraception research be it on an underpowered level due to lack of sufficient funding.
Before quitting, you might want to try a much smaller dose of 30mg twice a week along with about 375iu hCG twice a week on the same day as your testosterone shot. A lot of guys have a much stronger libido on 60mg per week than on 100mg per week. Don't get tied up with lab numbers, just go by how you feel.Wow that's going to take me
Wow . That's some read . I'll have a read through it all . I am due to get bloods in the next few weeks... This search for a libdio Is just not worth the way I'm feeling... Never ever felt good on trt m spent £1000`s looking for the libdio and I think it's time to stop
Thanks for the reply. I did try hCG when I first started trt 3 years ago and it made my anxiety go through the roof. I think at the time because my testosterone levels were still very low the the HCG was pushing my estradiol up so the the ratio was higher on the E2 side resulting in high anxiety. For me the only issue now with hCG is travelling as it has to be chilled... Obviously my testosterone levels are higher now than they were when I first started so hcg may be beneficialBefore quitting, you might want to try a much smaller dose of 30mg twice a week along with about 375iu hCG twice a week on the same day as your testosterone shot. A lot of guys have a much stronger libido on 60mg per week than on 100mg per week. Don't get tied up with lab numbers, just go by how you feel.
If you travel a lot, you could try Ovitrelle hCG, although it's not as effective as Pregnyl in my experience.
You may also feel good on just testosterone cypionate/enanthate at 30mg twice a week. Try it and let us know how you feel. I think the dose many guys start with is too high and then they end up quitting when they increase the dose and discover they feel even worse.
You may also feel good on just testosterone cypionate/enanthate at 30mg twice a week. Try it and let us know how you feel. I think the dose many guys start with is too high and then they end up quitting when they increase the dose and discover they feel even worse.
I dropped my test to 50 mg a week split between two injections . So 25 mg a shot. Just had full bloods done and will get those back next week. I've had headache for 13 days. Higher BP . Vision issues. More moody and irritable than normal and zero erectionsIf you travel a lot, you could try Ovitrelle hCG, although it's not as effective as Pregnyl in my experience.
You may also feel good on just testosterone cypionate/enanthate at 30mg twice a week. Try it and let us know how you feel. I think the dose many guys start with is too high and then they end up quitting when they increase the dose and discover they feel even worse.
So have you been taking 25mg twice a week over the last 13 days that you have been experiencing those negative side effects, or have you just begun 25mg twice a week?I dropped my test to 50 mg a week split between two injections . So 25 mg a shot. Just had full bloods done and will get those back next week. I've had headache for 13 days. Higher BP . Vision issues. More moody and irritable than normal and zero erections
Just begun the lowering of the test . All the symptoms were before. Just had my results back I'll attach pic of my free T .. shgb is high. It was high everyother day injection so lowered it two injections a week and took boron to lower the shgb and the shgb has gone up.... Also my TSH as at the very low end of the range .. could I have overactive thyroid as all my symptoms of low libido . Mood swings anxiety . Heart rate increase irritability all come under overactive thyroid.So have you been taking 25mg twice a week over the last 13 days that you have been experiencing those negative side effects, or have you just begun 25mg twice a week?
Boron is not all that effective in lowering SHBG in my experience and when it does work it's only very short term.
With high SHBG you're likely to feel better injecting once a week.
Another member sh1973 has tried all kinds of dosing protocols over the last 13 years and feels best on his current protocol of 60mg once a week.
It does look like you need to have your over active thyroid addressed. I hope some other members can offer you some helpful advice.
With high SHBG you're likely to feel better injecting once a week.
Another member sh1973 has tried all kinds of dosing protocols over the last 13 years and feels best on his current protocol of 60mg once a week.
It does look like you need to have your over active thyroid addressed. I hope some other members can offer you some helpful advice.
hCG Mixing Calculator
HCG Mixing Protocol Calculator
Similar threads
- Replies
- 101
- Views
- 7K
- Replies
- 25
- Views
- 4K
- Replies
- 43
- Views
- 9K
- Replies
- 5
- Views
- 566
- Replies
- 25
- Views
- 5K
TRT Hormone Predictor
Predict estradiol, DHT, and free testosterone levels based on total testosterone
⚠️ Medical Disclaimer
This tool provides predictions based on statistical models and should NOT replace professional medical advice. Always consult with your healthcare provider before making any changes to your TRT protocol.
ℹ️ Input Parameters
Normal range: 300-1000 ng/dL
Predicted Hormone Levels
Enter your total testosterone value to see predictions
Results will appear here after calculation
Understanding Your Hormones
Estradiol (E2)
A form of estrogen produced from testosterone. Important for bone health, mood, and libido. Too high can cause side effects; too low can affect well-being.
DHT
Dihydrotestosterone is a potent androgen derived from testosterone. Affects hair growth, prostate health, and masculinization effects.
Free Testosterone
The biologically active form of testosterone not bound to proteins. Directly available for cellular uptake and biological effects.
Scientific Reference
Lakshman KM, Kaplan B, Travison TG, Basaria S, Knapp PE, Singh AB, LaValley MP, Mazer NA, Bhasin S. The effects of injected testosterone dose and age on the conversion of testosterone to estradiol and dihydrotestosterone in young and older men. J Clin Endocrinol Metab. 2010 Aug;95(8):3955-64.
DOI: 10.1210/jc.2010-0102 | PMID: 20534765 | PMCID: PMC2913038
Online statistics
- Members online
- 5
- Guests online
- 220
- Total visitors
- 225
Totals may include hidden visitors.
Latest posts
-
-
-
The doctor who overturned medicine’s fear of testosterone
- Latest: Nelson Vergel
-
-
-
-
-
-
Going on Vacation and Will Miss My Testosterone Shots
- Latest: VacationMan
-