madman
Super Moderator
Dr. Dubin is a fellowship-trained urologist and andrologist focusing on men’s health. He cares for men with fertility problems, sexual issues (erectile dysfunction, premature ejaculation, delayed ejaculation, etc.), Peyronie’s disease, low testosterone, testicular pain and other problems involving men’s genitalia. He wants to help men understand that the issues they face are normal and help them find solutions that fit their lifestyle and life goals.
In addition to providing individualized patient care, he is also passionate about providing helpful information to the community. He co-hosts a podcast, “Man Up — A Doctor’s Guide to Men’s Health,” in which he discuss various men’s health topics.
- Why don’t men go to the doctor?
- Where do men get most of their sex ed from?
- Figuring out the difference between erections, orgasm, ejaculation (and refractory time) and desire.
- The five things you need to get a good erection.
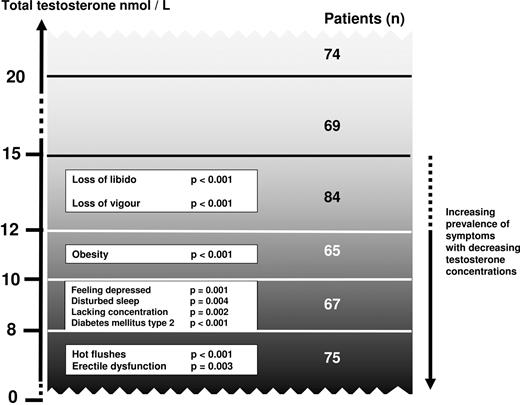
- The role of testosterone and libido and erections.
- Taking testosterone can cause infertility in 60% of men.
- Once you take Testosterone are you going to be on it forever?
- When a man goes to the doctor for Viagra, should the doctor ask about the partner?
- We need more people talking about intimacy without an erect penis.
- And if you are comfortable – what to do when you penis doesn’t work – I hear over and over about men being able to orgasm with a soft penis and I need some info on this! Are you the person? So many people think sex is over when the penis doesn’t work and I need someone to tackle this difficult topic.
- Dr. Dubin did a study looking at women getting blamed for their partner’s erectile dysfunction. 1 out of 7 women were blamed.
- Tips for when your male partner doesn’t want to talk about intimate issues.
- What is with products that make you make more semen?
- What is with penis enlarging procedures?
- Social media inaccuracies with men’s health – sperm retention!
- Does ejaculating decrease prostate cancer?
- Does vasectomy cause prostate cancer?
Chapters:
00:00 Introduction and Focus on Men's Sexual Health
02:10 Stigma and Hesitancy in Seeking Help
09:55 Understanding Sexual Function: Libido, Erections, Orgasm, and Ejaculation
16:47 Testosterone and Treatment Options
21:26 Considering Overall Well-being and Quality of Life
27:00 The Role of Communication and Education in Sexual Health
32:39 Expanding the Definition of Sex and Pleasure
34:07 Resources for Further Education and Support
34:54 Understanding and Addressing Erectile Dysfunction
55:52 Debunking Myths about Semen Retention and Penis Enlargement
59:47 The Importance of Communication in Sexual Health
01:03:02 The Relationship Between Ejaculation and Prostate Cancer
01:05:07 The Safety and Benefits of Vasectomy