Gianluca
Well-Known Member
Hello everybody. When I changed my protocol from Nebido to cypionate, I read that for those with low SHBG 12, the most recommended would be 20mg EOD, but with this protocol my hematocrit went up, BP increased, I had to do phlebotomy and ended up giving myself time to recover ferritin. I know that some people can resist and carry on with their protocol, but with these side effects I couldn't.
I read several articles and topics about TRT and hematocrit control, but many people did not finish the topics saying how they managed to control or ended up giving up TRT and that Undecanoate would be the ester that least caused erythrocytosis. My own experience also says this because I spent 1 year in Nebido and the hematocrit was controlled, but it is a very long ester and any adjustment is time consuming.
If you are sensitive like me to the cypionate, could you share your protocol and your experience of how you did it to control the hematocrit and follow the TRT? If you do phlebotomy, how do you replace the iron so that your ferritin is around 70?
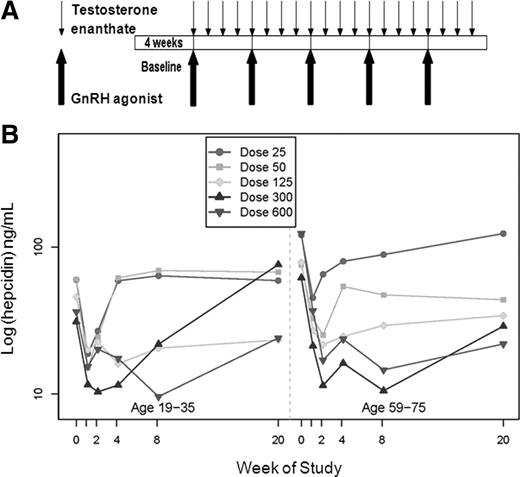
About the TRT protocol I read about the suppression of hepcidin and EPO and that what causes the increase in hematocrit would be more frequent doses such as DOE or ED since it would have little oscillation in the valley and thus our organism would spend more time producing RBCs and that the protocol, for example, 100 mg E7D with the cypionate the organism would stay longer ¨without producing¨ RBCs because there was a greater oscillation in the valley. How to reach the dose / frequency balance of the injections? What is your peak and your ideal valley? I'll leave one of the links where I read it if anyone wants to.

Does Injection Frequency Affect Hematocrit?
I switched from 76mg once a week to 38mg twice a week 2 months ago and my HCT did indeed rise a bit in last weeks blood. I only have 1 blood draw on the new protocol, but for whatever it’s worth RBC, Hemoglobin, Hematocrit, Platelets all rose higher than my previous 5 blood tests on various...forums.t-nation.com
As this subject has many variables and that each person reacts differently to the frequencies and doses of testosterone I decided to post this topic.
This forum has helped a lot around the world and this topic should help a lot of people who are starting in TRT and who sometimes give up due to lack of information.
Thank you for participating. Good weekend to everyone.
Just looking back at labs, i saw an increased in RBC with more frequent injections, especially everyday protocol. Always IM with the same dose.