You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
The Health Optimization Doctors RoundTable: High Hematocrit Not Important?
- Thread starter Systemlord
- Start date
T
tareload
Guest
- YouTube
Enjoy the videos and music you love, upload original content, and share it all with friends, family, and the world on YouTube.www.youtube.com
Simple question in the title of video.

Hematocrit drives Blood Viscosity- Does that Matter in Men on TRT? Effect of Altitude?
https://forums.t-nation.com/t/does-high-hematocrit-lead-to-complications-for-men-on-trt/268171/65 Update on my experiment with 325 mg/day of aspirin. Potent reduction in Hct while on TRT. One of the few supplements I've tried that really had a significant effect on Hct. Please consider the...
No glass test tubes here @RobRoy . Thanks for the videos and you can make another 100 hours of videos but it doesn't seem to sink in for you.

Hematocrit drives Blood Viscosity- Does that Matter in Men on TRT? Effect of Altitude?
https://forums.t-nation.com/t/does-high-hematocrit-lead-to-complications-for-men-on-trt/268171/65 Update on my experiment with 325 mg/day of aspirin. Potent reduction in Hct while on TRT. One of the few supplements I've tried that really had a significant effect on Hct. Please consider the...
As I always say read a lot understand little. That's our name for you inside our circles. The woke TRT movement is in full affect with you read a lot. I guess you missed the part where we talk about the beneficial effects that testosterone has on the vasculature. You can't use baseline studies on him adequate and apply that to men on testosterone. You can't apply laboratory studies two men on testosterone. None of the causes of secondary erythrocytosis have an increase risk of heart attack strokes or blood clots and that includes living at high altitude, COPD, and sleep apnea for instance. Testosterone has also never been shown to increase a man's risk of heart attack strokes or blood clots despite an increase in hematocrit being the most common side effect from testosterone. Testosterone has multiple beneficial effects on vascular reactivity. You should've been at the Androgen Society meeting this year where it was discussed in detail and stated out loud that the increase in hematocrit does not cause harm. Just ask Nelson he was there. So now you're gonna have to include Abraham Morgenthaler as a target in your woke TRT movement. Yes Abraham Morgenthaler stated it out loud that the increase in hematocrit has never been shown to cause harm and that the hematocrit cut off is an arbitrary number not based on data. I actually have his exact words taped. Multiple leaders in the industry were also there and felt the same way.
But the best way to prove your hypothesis that the increase in Hct on testosterone could cause harm is to actually give testosterone to men raise their hematocrit and see if it causes harm. Oh wait a minute that's been done for 85 years and guess what it's never caused harm. It's been abused for decades by men and yet has never caused harm. The first couple of decades that mean we're given testosterone there were no lab test so they were given how doses of testosterone or what you would consider high-dose which would be 200 mg and guess what no harm was done despite them having an increase Hct. I guess you also think testosterone causes prostate cancer or worsens it as well don't you?
You may can talk around the uninformed on a forum but it's obvious you have absolutely zero clinical experience but you want to attack those that have literally decades of clinical experience and understand the actual literature.
I've asked you over and over and over again I'm gonna ask you one last time. Provide one single study where testosterone caused an increase in heart attack strokes or blood clots. Provide any study that you would like that raising the hematocrit with testosterone caused harm.
I guess you're also gonna tell us that if you live at altitude you are also an increased risk due to the high hematocrit that you get. Are you gonna tell us that too or you just want to continue your woke TRT movement?
Abraham Morgenthaler the father of testosterone therapy and prostate cancer disagrees with you read a lot.
" In experimental studies using rigid glass viscometers or cone-plate viscometers there is a logarithmic increase in viscosity with increasing hematocrit. It is inappropriate to correlate these in vitro viscosity readings to what occurs to flowing blood through tiny distensible vessels in vivo. In other words, viscometer measures in these experiments do not translate to human blood vessels. Firstly, the flow through these narrow blood vessels is rapid (high shear rate), which in a non-Newtonian fluid such as blood causes a marked decrease in viscosity. Second, blood flowing through these narrow channels is axial with a central core of packed red blood cells sliding over a peripheral layer of lubricating low viscosity plasma. With a secondary erythrocytosis there is an increase in blood volume which enlarges the vascular bed, decreases peripheral resistance and increases cardiac output. Therefore, in a secondary erythrocytosis optimal oxygen transport with increased blood volume occurs at a higher hematocrit value than with a normal blood volume. A moderate increase in hematocrit may be beneficial despite the increased viscosity" (this is straight from Williams hematology which you conveniently left out)
Testosterone also exerts multiple beneficial effects on the vasculature and its components which may protect against thrombosis. In other words testosterone has positive effects on vascular reactivity.
Testosterone is a vasodilator and increases nitric oxide
T decreases plasma concentrations of pro coagulatory substances
T improves erythrocyte membrane lipid composition and fluidity
T increases red blood cell deformability
T reduces levels of lipoprotein a
The brightest researchers in the world including Abraham Morgenthaler disagree with you read a lot. It gets so tiring asking you to provide an actual study showing any harm in men using testosterone or raising Hct with testosterone. I guess you also missed the part of the video where the upper limit of hematocrit is an arbitrary number. It's not based on any data that shows harm when you go above it. It's just an arbitrary number. Dr. Morgenthaler pointed this out very clearly at the androgen society meeting and Glenn Cunningham who wrote the guidelines for testosterone therapy for the endocrine Society stated they only picked 54% because they had to pick a number and it seemed like a good number but there wasn't any data that factored into the decision. Once again let's quote Dr. Neal Rouzier "in medicine if we say that it might it means that it doesn't because if it did we would say that it does. Testosterone has been used for almost 100 years and it has not caused harm... but read a lot thinks that it can. I'll ask you a different question, are you also afraid of the dark?

But the best way to prove your hypothesis that the increase in Hct on testosterone could cause harm is to actually give testosterone to men raise their hematocrit and see if it causes harm. Oh wait a minute that's been done for 85 years and guess what it's never caused harm. It's been abused for decades by men and yet has never caused harm. The first couple of decades that mean we're given testosterone there were no lab test so they were given how doses of testosterone or what you would consider high-dose which would be 200 mg and guess what no harm was done despite them having an increase Hct. I guess you also think testosterone causes prostate cancer or worsens it as well don't you?
You may can talk around the uninformed on a forum but it's obvious you have absolutely zero clinical experience but you want to attack those that have literally decades of clinical experience and understand the actual literature.
I've asked you over and over and over again I'm gonna ask you one last time. Provide one single study where testosterone caused an increase in heart attack strokes or blood clots. Provide any study that you would like that raising the hematocrit with testosterone caused harm.
I guess you're also gonna tell us that if you live at altitude you are also an increased risk due to the high hematocrit that you get. Are you gonna tell us that too or you just want to continue your woke TRT movement?
Abraham Morgenthaler the father of testosterone therapy and prostate cancer disagrees with you read a lot.
" In experimental studies using rigid glass viscometers or cone-plate viscometers there is a logarithmic increase in viscosity with increasing hematocrit. It is inappropriate to correlate these in vitro viscosity readings to what occurs to flowing blood through tiny distensible vessels in vivo. In other words, viscometer measures in these experiments do not translate to human blood vessels. Firstly, the flow through these narrow blood vessels is rapid (high shear rate), which in a non-Newtonian fluid such as blood causes a marked decrease in viscosity. Second, blood flowing through these narrow channels is axial with a central core of packed red blood cells sliding over a peripheral layer of lubricating low viscosity plasma. With a secondary erythrocytosis there is an increase in blood volume which enlarges the vascular bed, decreases peripheral resistance and increases cardiac output. Therefore, in a secondary erythrocytosis optimal oxygen transport with increased blood volume occurs at a higher hematocrit value than with a normal blood volume. A moderate increase in hematocrit may be beneficial despite the increased viscosity" (this is straight from Williams hematology which you conveniently left out)
Testosterone also exerts multiple beneficial effects on the vasculature and its components which may protect against thrombosis. In other words testosterone has positive effects on vascular reactivity.
Testosterone is a vasodilator and increases nitric oxide
T decreases plasma concentrations of pro coagulatory substances
T improves erythrocyte membrane lipid composition and fluidity
T increases red blood cell deformability
T reduces levels of lipoprotein a
The brightest researchers in the world including Abraham Morgenthaler disagree with you read a lot. It gets so tiring asking you to provide an actual study showing any harm in men using testosterone or raising Hct with testosterone. I guess you also missed the part of the video where the upper limit of hematocrit is an arbitrary number. It's not based on any data that shows harm when you go above it. It's just an arbitrary number. Dr. Morgenthaler pointed this out very clearly at the androgen society meeting and Glenn Cunningham who wrote the guidelines for testosterone therapy for the endocrine Society stated they only picked 54% because they had to pick a number and it seemed like a good number but there wasn't any data that factored into the decision. Once again let's quote Dr. Neal Rouzier "in medicine if we say that it might it means that it doesn't because if it did we would say that it does. Testosterone has been used for almost 100 years and it has not caused harm... but read a lot thinks that it can. I'll ask you a different question, are you also afraid of the dark?
Last edited:
T
tareload
Guest
Shall I post you a pdf of the TRAVERSE study or is that a flawed study? Or did they not get those TT/FT levels high enough? Yeah they got those guys up to sissy levels, I know.As I always say read a lot understand little. That's our name for you inside our circles. The woke TRT movement is in full affect with you read a lot. I guess you missed the part where we talk about the beneficial effects that testosterone has on the vasculature. You can't use baseline studies on him adequate and apply that to men on testosterone. You can't apply laboratory studies two men on testosterone. None of the causes of secondary erythrocytosis have an increase risk of heart attack strokes or blood clots and that includes living at high altitude, COPD, and sleep apnea for instance. Testosterone has also never been shown to increase a man's risk of heart attack strokes or blood clots despite an increase in hematocrit being the most common side effect from testosterone. Testosterone has multiple beneficial effects on vascular reactivity. You should've been at the Androgen Society meeting this year where it was discussed in detail and stated out loud that the increase in hematocrit does not cause harm. Just ask Nelson he was there. So now you're gonna have to include Abraham Morgenthaler as a target in your woke TRT movement. Yes Abraham Morgenthaler stated it out loud that the increase in hematocrit has never been shown to cause harm and that the hematocrit cut off is an arbitrary number not based on data. I actually have his exact words taped. Multiple leaders in the industry were also there and felt the same way.
But the best way to prove your hypothesis that the increase in Hct on testosterone could cause harm is to actually give testosterone to men raise their hematocrit and see if it causes harm. Oh wait a minute that's been done for 85 years and guess what it's never caused harm. It's been abused for decades by men and yet has never caused harm. The first couple of decades that mean we're given testosterone there were no lab test so they were given how doses of testosterone or what you would consider high-dose which would be 200 mg and guess what no harm was done despite them having an increase Hct. I guess you also think testosterone causes prostate cancer or worsens it as well don't you?
You may can talk around the uninformed on a forum but it's obvious you have absolutely zero clinical experience but you want to attack those that have literally decades of clinical experience and understand the actual literature.
I've asked you over and over and over again I'm gonna ask you one last time. Provide one single study where testosterone caused an increase in heart attack strokes or blood clots. Provide any study that you would like that raising the hematocrit with testosterone caused harm.
I guess you're also gonna tell us that if you live at altitude you are also an increased risk due to the high hematocrit that you get. Are you gonna tell us that too or you just want to continue your woke TRT movement?
Abraham Morgenthaler the father of testosterone therapy and prostate cancer disagrees with you read a lot.
" In experimental studies using rigid glass viscometers or cone-plate viscometers there is a logarithmic increase in viscosity with increasing hematocrit. It is inappropriate to correlate these in vitro viscosity readings to what occurs to flowing blood through tiny distensible vessels in vivo. In other words, viscometer measures in these experiments do not translate to human blood vessels. Firstly, the flow through these narrow blood vessels is rapid (high shear rate), which in a non-Newtonian fluid such as blood causes a marked decrease in viscosity. Second, blood flowing through these narrow channels is axial with a central core of packed red blood cells sliding over a peripheral layer of lubricating low viscosity plasma. With a secondary erythrocytosis there is an increase in blood volume which enlarges the vascular bed, decreases peripheral resistance and increases cardiac output. Therefore, in a secondary erythrocytosis optimal oxygen transport with increased blood volume occurs at a higher hematocrit value than with a normal blood volume. A moderate increase in hematocrit may be beneficial despite the increased viscosity" (this is straight from Williams hematology which you conveniently left out)
Testosterone also exerts multiple beneficial effects on the vasculature and its components which may protect against thrombosis. In other words testosterone has positive effects on vascular reactivity.
Testosterone is a vasodilator and increases nitric oxide
T decreases plasma concentrations of pro coagulatory substances
T improves erythrocyte membrane lipid composition and fluidity
T increases red blood cell deformability
T reduces levels of lipoprotein a
The brightest researchers in the world including Abraham Morgenthaler disagree with you read a lot. It gets so tiring asking you to provide an actual study showing any harm in men using testosterone or raising Hct with testosterone. I guess you also missed the part of the video where the upper limit of hematocrit is an arbitrary number. It's not based on any data that shows harm when you go above it. It's just an arbitrary number. Dr. Morgenthaler pointed this out very clearly at the androgen society meeting and Glenn Cunningham who wrote the guidelines for testosterone therapy for the endocrine Society stated they only picked 54% because they had to pick a number and it seemed like a good number but there wasn't any data that factored into the decision. Once again let's quote Dr. Neal Rouzier "in medicine if we say that it might it means that it doesn't because if it did we would say that it does. Testosterone has been used for almost 100 years and it has not caused harm... but read a lot thinks that it can. I'll ask you a different question, are you also afraid of the dark?
View attachment 33604View attachment 33605
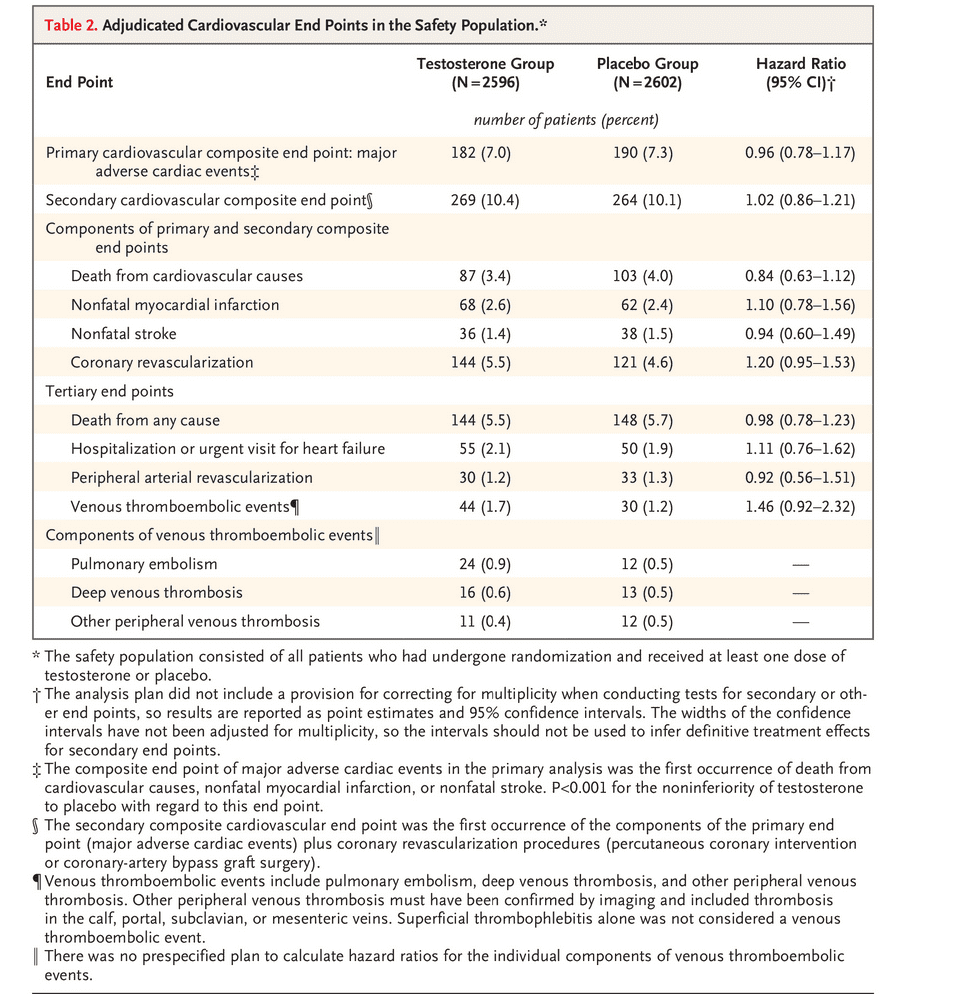
Woke TRT? You just keep getting funnier. Thank you for the entertainment. Call Dr. Scott and read him the study as a bedtime story. LoL.
Lemme guess, that AFIB finding and arythmmia is bullshit as well? Ignore symphathic modulation much, do you?
They even took out the dudes with over 54% Hct from the treatment arm haha.
I watched the whole video BTW. Keep waving your hands or try being intellectually honest for a refreshing change.
Get Danny Bossa over here as well and you can all apologize to me. He had an excuse being a civilian entertainer... What is your excuse?
You can appeal to authority all you want good Doctor and I am glad @Nelson Vergel was there at the meeting with you. You and your circle have lots to discuss now. Can't wait to hear your plans for TRAVERSE II with two treatment arms (20 to 30 ng/dl FT vs 30 to 40 ng/dl FT vs placebo). That's going to be a lot of cream. What do you think will happen? Make sure you don't remove the guys running over 54% Hct as well (just more oxygen in the blood, righr?).
Last edited by a moderator:
Guided_by_Voices
Well-Known Member
Why is Hematocrit even worth arguing about since blood donation (which people should be doing anyway for multiple reasons) substantially removes the issue for most men? I know there could be periods pre-donation where it has crept up but it seems like your discussion assumes chronic "elevation" (whatever that may be) and that should rarely be the case.
T
tareload
Guest
Blood donation? Heresy. Why would anyone do that when the Good Doc has told us over and over again that secondary erythrocytosis with "TRT" or TRT is completely harmless. Plus tesosterone is good for you. You can't hurt a man giving him testosterone, right Doc?

 forums.t-nation.com
forums.t-nation.com

 forums.t-nation.com
forums.t-nation.com

E2 Climbing on Same Test Dose + Heartburn
Read a lot tell me how you don’t know what hormone optimization is without telling me you don’t know what hormone optimization is. I understand you with your medical problems and atrial fibrillation from utilizing anabolic steroids do you want men to have optimal testosterone levels. I think...
 forums.t-nation.com
forums.t-nation.com

E2 Climbing on Same Test Dose + Heartburn
But read a lot but you don’t have is any clinical experience. You have zero clinical experience with men. I have over 20 years of clinical experience with men. We see what supraphysiological levels do for men. Let’s define that by today’s standards and that is anything over 916 ng/dL…ridiculous...
 forums.t-nation.com
forums.t-nation.com
T
tareload
Guest
Get that video camera warmed up...
Link: TRAVERSE STUDY WITH ANDROGEL
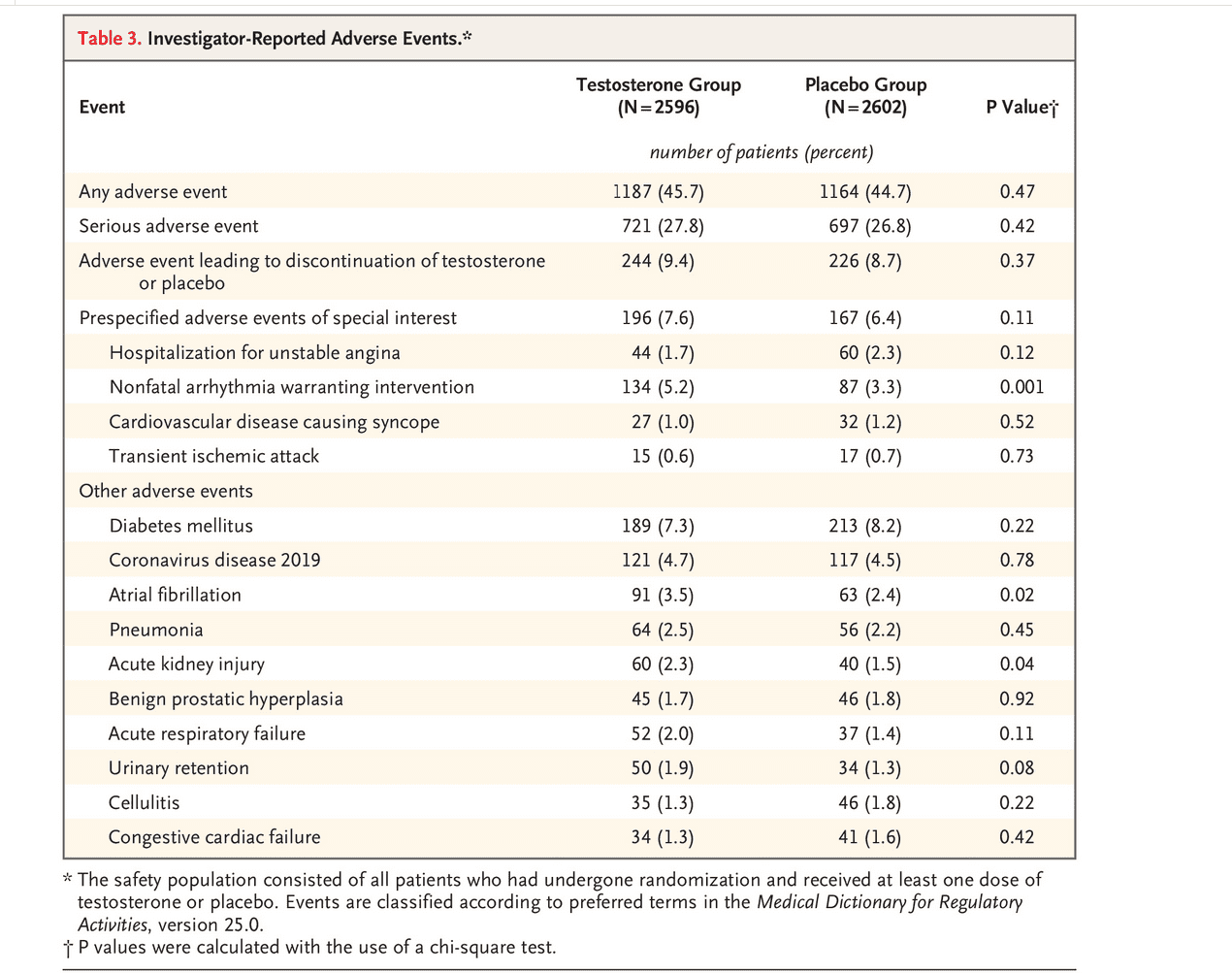
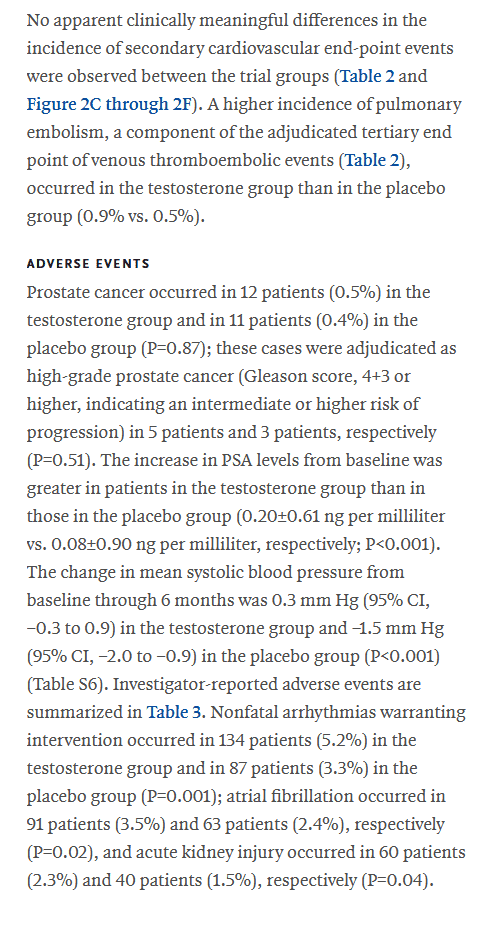
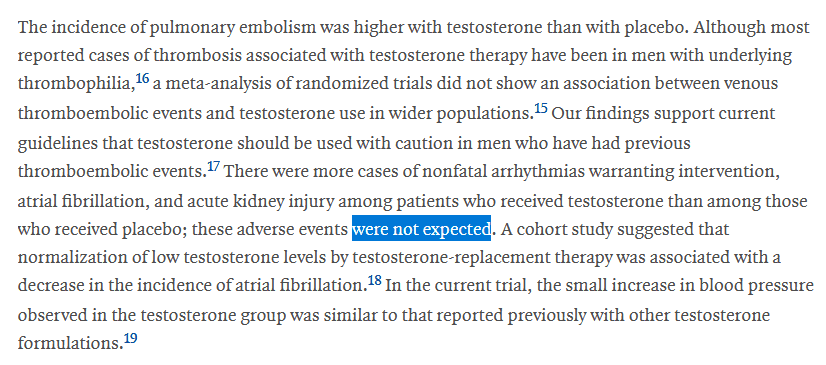
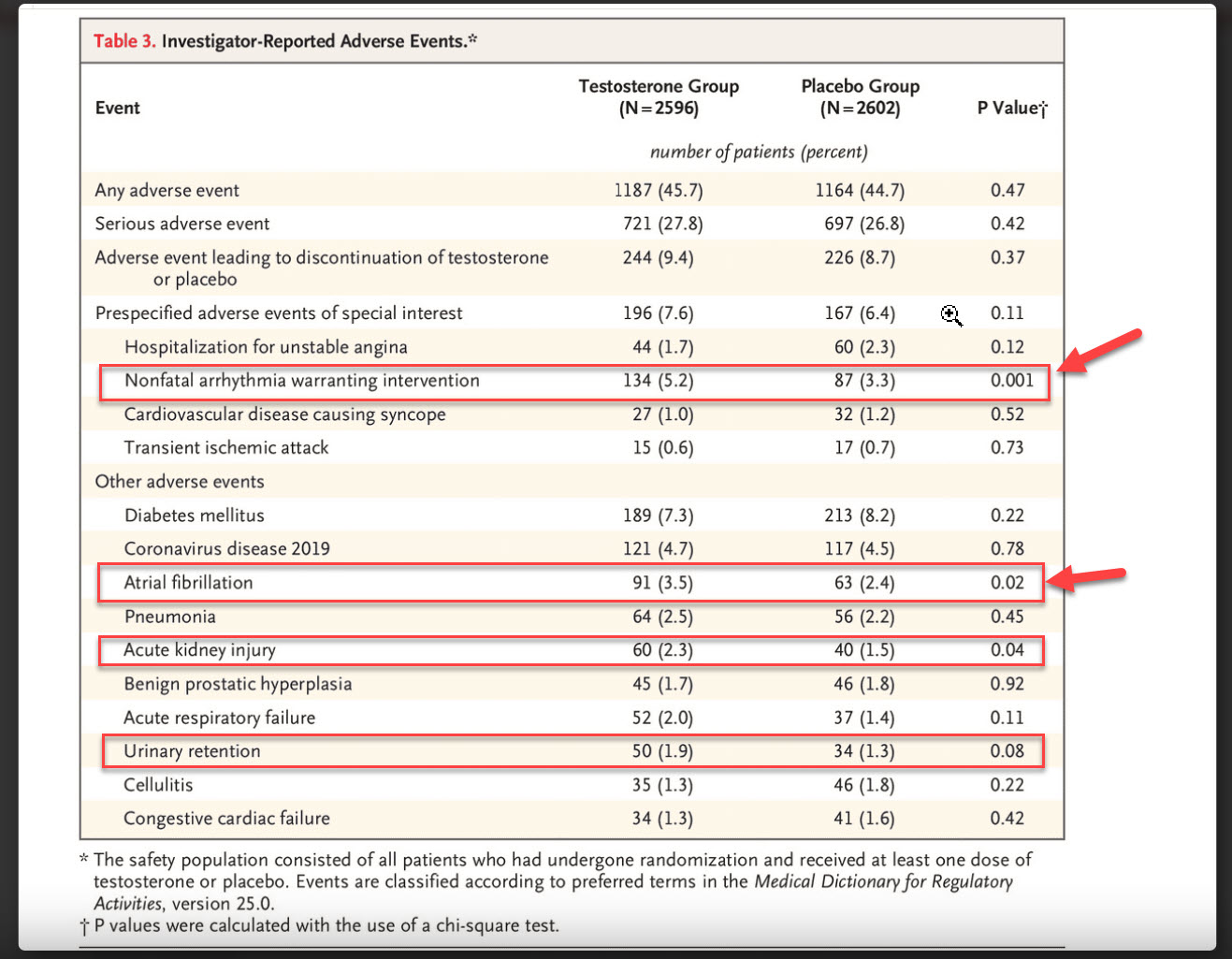
This Androgel study's results showing a p<0.001 and 0.02 for arrythmia and atrial fibrillation may be explained by:

 www.excelmale.com
www.excelmale.com
Looks harmless [joking]. Giving men a man sized dose of testosterone is probably even more harmless LOL.
Cue the Jay laugh track.

Link: TRAVERSE STUDY WITH ANDROGEL
This Androgel study's results showing a p<0.001 and 0.02 for arrythmia and atrial fibrillation may be explained by:

Impact of Hemoglobin Levels and Their Dynamic Changes on the Risk of Atrial Fibrillation: A Nationwide Population-Based Study
Abstract Anemia is a risk factor for cardiovascular disease, but its impact on new-onset atrial fibrillation (AF) is unclear. In this study, we investigated the effect of hemoglobin (Hb) levels and their changes on the risk of AF development in the general population of Korea. We retrospectively...
Looks harmless [joking]. Giving men a man sized dose of testosterone is probably even more harmless LOL.
Cue the Jay laugh track.

Last edited by a moderator:
Nelson Vergel
Founder, ExcelMale.com
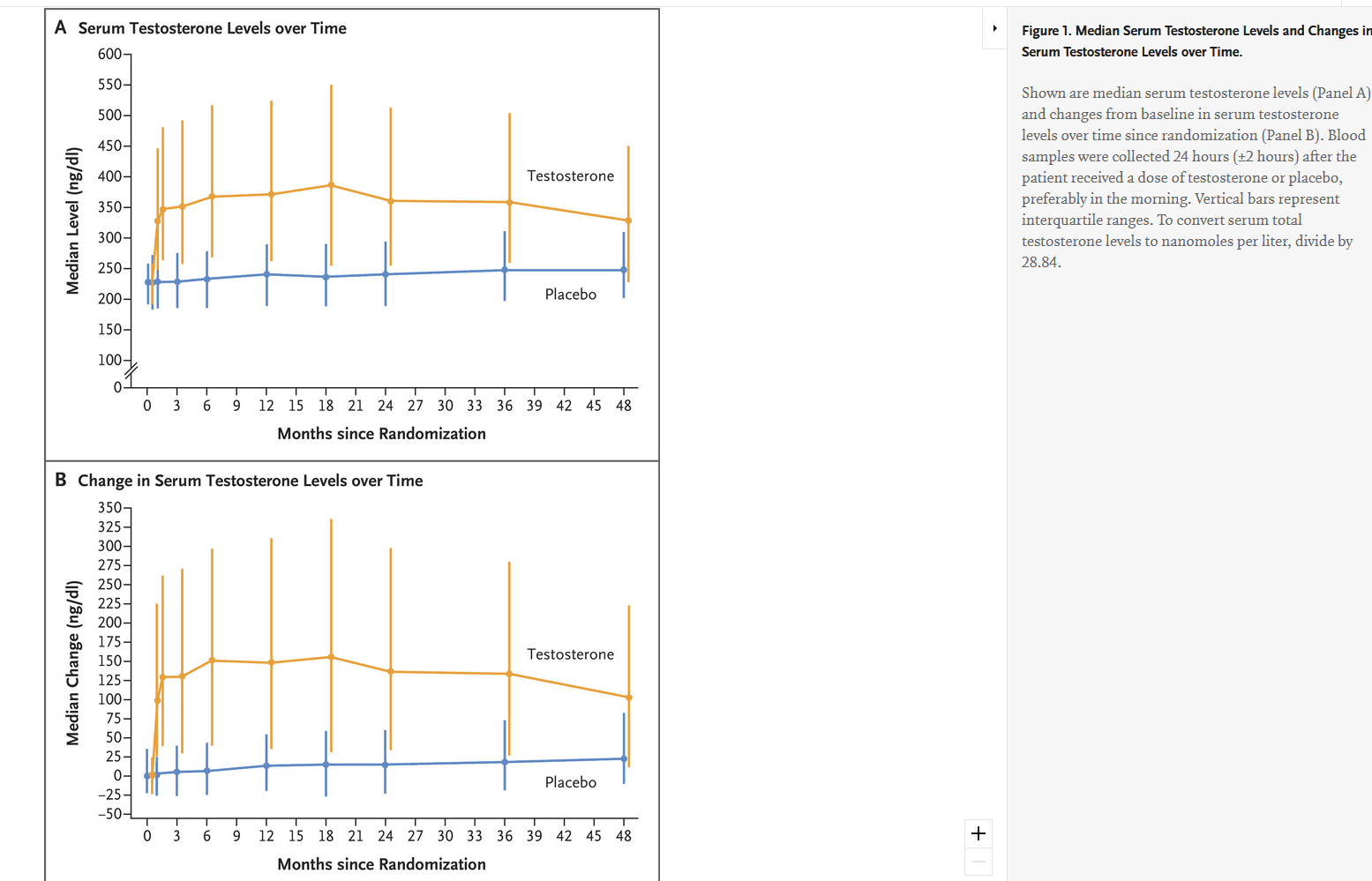
This study was done with T gels and max hematocrit was 52
Nelson Vergel
Founder, ExcelMale.com
Nelson Vergel
Founder, ExcelMale.com
T
tareload
Guest
Nelson Vergel
Founder, ExcelMale.com
From Ramasamy' study:
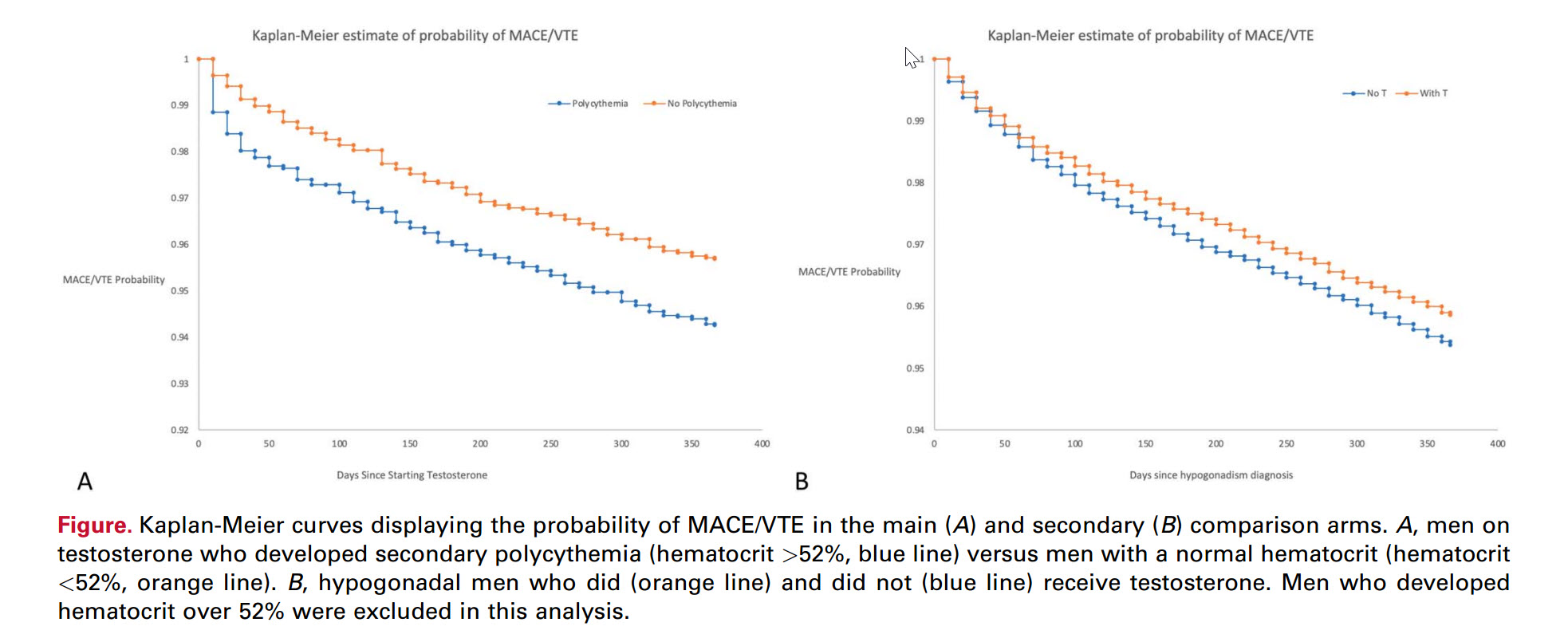
We demonstrated that developing secondary polycythemia while receiving TT, defined as a hematocrit over 52%, was associated with increased risk of developing MACE and VTE during the first year of therapy. TT itself, in the absence of polycythemia, did not appear to increase risk of MACE/VTE in hypogonadal men. To our knowledge, this is the first study to establish secondary polycythemia from TT as an independent risk factor for MACE/VTE using a specific hematocrit-based cutoff.
We used a large national database to answer this question, hypothesizing that real-world data would be best suited to address this issue. Men with high baseline hematocrit are often excluded from randomized trials, and in clinical practice pre-treatment blood work is often not done, and guidelines are frequently not followed.20,21 This leaves a large population of men using TT who are not represented by RCTs. Our findings are somewhat supported by prior literature.
The TOM (Testosterone in Older Men with Sarcopenia) trial, an RCT that was stopped early due to increased risk of cardiovascular adverse events, included older men with a high incidence of comorbid conditions.22 While this trial only included 209 men, their demographic information is similar in nature to our study, which included a large proportion of men with comorbid conditions. Like most RCTs on testosterone, the TOM trial did not report hematocrit values in those men with cardiovascular events. One systematic review on this topic did not find overall increased cardiovascular risk, however they did find an increased event rate in the first 12 months of therapy, supporting our window of 1 year for evaluation of MACE/VTE.23
Another review reinforced the value of using large databases in answering this question, highlighting that all published RCTs on this topic are underpowered to assess any association with treatment and cardiovascular outcomes.24
This will hopefully be addressed by the TRAVERSE (Testosterone Replacement Therapy for Assessment of Long-term Vascular Events and Efficacy ResponSE in Hypogonadal Men) trial (NCT03518034), however polycythemia or hematocrit-based adverse events are not listed as an outcome.It is well established that TT increases the risk of secondary polycythemia,25 with higher rates in longer-acting modalities and lower rates in shorter-acting modalities.16 Multiple national guidelines use elevation in hematocrit as a trigger to stop or change TT in men.
TT cessation triggers include 55% from Canadian guidelines,9 54% from endocrine society guidelines and European urology guidelines,5,26 and between 50%–54% from American urological guidelines.10 While the rationale for these cutoffs is not cited in these guidelines, they appear to come from the Framingham heart study, which found an increase in adverse cardiovascular outcomes with a hematocrit of 49% or higher.8 These findings were confirmed in a more recent prospective cohort study, which found an increased rate of overall and cardiovascular-related mortality once hematocrit entered the range of 50%–54%.27 Neither of these studies specifically studied men on testosterone, and thus the currently existing hematocrit cutoffs amongst TT users is arbitrary. For the purposes of our study, we chose a cutoff of 52%, reflecting other published literature, and to ensure a relatively large comparator arm.10,16
The strengths of this study include its use of a large multi-institutional database and being a real-world snapshot of the effects of TT in a U.S. cohort. There is increasing evidence that nonrandomized evidence from large databases can accurately emulate a large-scale RCT, lending validity to these results.28 Detailed propensity-score matching increased the validity of our findings. Lastly, our sensitivity analyses, and analysis of TT-naïve men, support the role of polycythemia as an independent, critical factor in the development of MACE/VTE.
Limitations include the inability to segregate results by type of testosterone prescription. In addition, a large percentage of the men included are Caucasian (86%), and the matched populations have a relatively high comorbidity index, limiting the generalizability of the findings to minorities and healthy individuals. Furthermore, we were not able to match the 2 groups by baseline hematocrit, as the men in the polycythemia group had a higher baseline hematocrit.
Therefore, we cannot definitively determine whether the increased risk of MACE/VTE is due to hematocrit reaching 52% or due to men with higher baseline hematocrit starting TT. Regardless, the baseline hematocrit in the polycythemia group was 47.4%, which according to U.S., Canadian and European guidelines does not warrant further investigation before starting TT.
Lastly, due to the limitations of the TriNetX database, we were unable to analyze hematocrit as a continuous variable.Regardless of these limitations, this study lends prescribers a practical approach to informing about risks of TT, and reinforces existing guideline practices of checking hematocrit prior to prescribing.5 It also provides a hematocrit-based cutoff that comes directly from a population of men using TT, and can hopefully allow future guideline statements to remain consistent across recommendations. Future studies that aim to assess cardiovascular outcomes in men on testosterone (such as the ongoing TRAVERSE study, NCT03518034) should perform detailed analysis on hematocrit change to investigate this as a possible association.
We demonstrated that developing secondary polycythemia while receiving TT, defined as a hematocrit over 52%, was associated with increased risk of developing MACE and VTE during the first year of therapy. TT itself, in the absence of polycythemia, did not appear to increase risk of MACE/VTE in hypogonadal men. To our knowledge, this is the first study to establish secondary polycythemia from TT as an independent risk factor for MACE/VTE using a specific hematocrit-based cutoff.
We used a large national database to answer this question, hypothesizing that real-world data would be best suited to address this issue. Men with high baseline hematocrit are often excluded from randomized trials, and in clinical practice pre-treatment blood work is often not done, and guidelines are frequently not followed.20,21 This leaves a large population of men using TT who are not represented by RCTs. Our findings are somewhat supported by prior literature.
The TOM (Testosterone in Older Men with Sarcopenia) trial, an RCT that was stopped early due to increased risk of cardiovascular adverse events, included older men with a high incidence of comorbid conditions.22 While this trial only included 209 men, their demographic information is similar in nature to our study, which included a large proportion of men with comorbid conditions. Like most RCTs on testosterone, the TOM trial did not report hematocrit values in those men with cardiovascular events. One systematic review on this topic did not find overall increased cardiovascular risk, however they did find an increased event rate in the first 12 months of therapy, supporting our window of 1 year for evaluation of MACE/VTE.23
Another review reinforced the value of using large databases in answering this question, highlighting that all published RCTs on this topic are underpowered to assess any association with treatment and cardiovascular outcomes.24
This will hopefully be addressed by the TRAVERSE (Testosterone Replacement Therapy for Assessment of Long-term Vascular Events and Efficacy ResponSE in Hypogonadal Men) trial (NCT03518034), however polycythemia or hematocrit-based adverse events are not listed as an outcome.It is well established that TT increases the risk of secondary polycythemia,25 with higher rates in longer-acting modalities and lower rates in shorter-acting modalities.16 Multiple national guidelines use elevation in hematocrit as a trigger to stop or change TT in men.
TT cessation triggers include 55% from Canadian guidelines,9 54% from endocrine society guidelines and European urology guidelines,5,26 and between 50%–54% from American urological guidelines.10 While the rationale for these cutoffs is not cited in these guidelines, they appear to come from the Framingham heart study, which found an increase in adverse cardiovascular outcomes with a hematocrit of 49% or higher.8 These findings were confirmed in a more recent prospective cohort study, which found an increased rate of overall and cardiovascular-related mortality once hematocrit entered the range of 50%–54%.27 Neither of these studies specifically studied men on testosterone, and thus the currently existing hematocrit cutoffs amongst TT users is arbitrary. For the purposes of our study, we chose a cutoff of 52%, reflecting other published literature, and to ensure a relatively large comparator arm.10,16
The strengths of this study include its use of a large multi-institutional database and being a real-world snapshot of the effects of TT in a U.S. cohort. There is increasing evidence that nonrandomized evidence from large databases can accurately emulate a large-scale RCT, lending validity to these results.28 Detailed propensity-score matching increased the validity of our findings. Lastly, our sensitivity analyses, and analysis of TT-naïve men, support the role of polycythemia as an independent, critical factor in the development of MACE/VTE.
Limitations include the inability to segregate results by type of testosterone prescription. In addition, a large percentage of the men included are Caucasian (86%), and the matched populations have a relatively high comorbidity index, limiting the generalizability of the findings to minorities and healthy individuals. Furthermore, we were not able to match the 2 groups by baseline hematocrit, as the men in the polycythemia group had a higher baseline hematocrit.
Therefore, we cannot definitively determine whether the increased risk of MACE/VTE is due to hematocrit reaching 52% or due to men with higher baseline hematocrit starting TT. Regardless, the baseline hematocrit in the polycythemia group was 47.4%, which according to U.S., Canadian and European guidelines does not warrant further investigation before starting TT.
Lastly, due to the limitations of the TriNetX database, we were unable to analyze hematocrit as a continuous variable.Regardless of these limitations, this study lends prescribers a practical approach to informing about risks of TT, and reinforces existing guideline practices of checking hematocrit prior to prescribing.5 It also provides a hematocrit-based cutoff that comes directly from a population of men using TT, and can hopefully allow future guideline statements to remain consistent across recommendations. Future studies that aim to assess cardiovascular outcomes in men on testosterone (such as the ongoing TRAVERSE study, NCT03518034) should perform detailed analysis on hematocrit change to investigate this as a possible association.
CONCLUSION
Men using TT should be aware that they are at a higher risk for MACE/VTE if their hematocrit reaches or exceeds 52% during the first year of therapy. This is especially relevant in men with cardiovascular comorbidities. Hematocrit-based cutoffs should be incorporated into the outcomes of future RCTs investigating MACE/VTE and TT.Nelson Vergel
Founder, ExcelMale.com
The TRAVERSE study they mentioned was presented recently. However, it only included men on Androgel, not injections. High hematocrit was not as common, so it is a moot subject for most men on this forum on T injections running high T blood levels and hematocrit over 52.
See post 9 above.
See post 9 above.
T
tareload
Guest
From Ramasamy' study:
We demonstrated that developing secondary polycythemia while receiving TT, defined as a hematocrit over 52%, was associated with increased risk of developing MACE and VTE during the first year of therapy. TT itself, in the absence of polycythemia, did not appear to increase risk of MACE/VTE in hypogonadal men. To our knowledge, this is the first study to establish secondary polycythemia from TT as an independent risk factor for MACE/VTE using a specific hematocrit-based cutoff.
We used a large national database to answer this question, hypothesizing that real-world data would be best suited to address this issue. Men with high baseline hematocrit are often excluded from randomized trials, and in clinical practice pre-treatment blood work is often not done, and guidelines are frequently not followed.20,21 This leaves a large population of men using TT who are not represented by RCTs. Our findings are somewhat supported by prior literature.
The TOM (Testosterone in Older Men with Sarcopenia) trial, an RCT that was stopped early due to increased risk of cardiovascular adverse events, included older men with a high incidence of comorbid conditions.22 While this trial only included 209 men, their demographic information is similar in nature to our study, which included a large proportion of men with comorbid conditions. Like most RCTs on testosterone, the TOM trial did not report hematocrit values in those men with cardiovascular events. One systematic review on this topic did not find overall increased cardiovascular risk, however they did find an increased event rate in the first 12 months of therapy, supporting our window of 1 year for evaluation of MACE/VTE.23
Another review reinforced the value of using large databases in answering this question, highlighting that all published RCTs on this topic are underpowered to assess any association with treatment and cardiovascular outcomes.24
This will hopefully be addressed by the TRAVERSE (Testosterone Replacement Therapy for Assessment of Long-term Vascular Events and Efficacy ResponSE in Hypogonadal Men) trial (NCT03518034), however polycythemia or hematocrit-based adverse events are not listed as an outcome.It is well established that TT increases the risk of secondary polycythemia,25 with higher rates in longer-acting modalities and lower rates in shorter-acting modalities.16 Multiple national guidelines use elevation in hematocrit as a trigger to stop or change TT in men.
TT cessation triggers include 55% from Canadian guidelines,9 54% from endocrine society guidelines and European urology guidelines,5,26 and between 50%–54% from American urological guidelines.10 While the rationale for these cutoffs is not cited in these guidelines, they appear to come from the Framingham heart study, which found an increase in adverse cardiovascular outcomes with a hematocrit of 49% or higher.8 These findings were confirmed in a more recent prospective cohort study, which found an increased rate of overall and cardiovascular-related mortality once hematocrit entered the range of 50%–54%.27 Neither of these studies specifically studied men on testosterone, and thus the currently existing hematocrit cutoffs amongst TT users is arbitrary. For the purposes of our study, we chose a cutoff of 52%, reflecting other published literature, and to ensure a relatively large comparator arm.10,16
The strengths of this study include its use of a large multi-institutional database and being a real-world snapshot of the effects of TT in a U.S. cohort. There is increasing evidence that nonrandomized evidence from large databases can accurately emulate a large-scale RCT, lending validity to these results.28 Detailed propensity-score matching increased the validity of our findings. Lastly, our sensitivity analyses, and analysis of TT-naïve men, support the role of polycythemia as an independent, critical factor in the development of MACE/VTE.
Limitations include the inability to segregate results by type of testosterone prescription. In addition, a large percentage of the men included are Caucasian (86%), and the matched populations have a relatively high comorbidity index, limiting the generalizability of the findings to minorities and healthy individuals. Furthermore, we were not able to match the 2 groups by baseline hematocrit, as the men in the polycythemia group had a higher baseline hematocrit.
Therefore, we cannot definitively determine whether the increased risk of MACE/VTE is due to hematocrit reaching 52% or due to men with higher baseline hematocrit starting TT. Regardless, the baseline hematocrit in the polycythemia group was 47.4%, which according to U.S., Canadian and European guidelines does not warrant further investigation before starting TT.
Lastly, due to the limitations of the TriNetX database, we were unable to analyze hematocrit as a continuous variable.Regardless of these limitations, this study lends prescribers a practical approach to informing about risks of TT, and reinforces existing guideline practices of checking hematocrit prior to prescribing.5 It also provides a hematocrit-based cutoff that comes directly from a population of men using TT, and can hopefully allow future guideline statements to remain consistent across recommendations. Future studies that aim to assess cardiovascular outcomes in men on testosterone (such as the ongoing TRAVERSE study, NCT03518034) should perform detailed analysis on hematocrit change to investigate this as a possible association.
CONCLUSION
Men using TT should be aware that they are at a higher risk for MACE/VTE if their hematocrit reaches or exceeds 52% during the first year of therapy. This is especially relevant in men with cardiovascular comorbidities. Hematocrit-based cutoffs should be incorporated into the outcomes of future RCTs investigating MACE/VTE and TT.
Look....I even save time for @RobRoy

Does Estrogen Make Me Fat? What about Fertility?
Hey Tareload, I spoke specifically with the author of this article in Florida just two months ago. I had a very specific conversation with doctor Ramasamy after he presented this article. Guess what? His statement was that he doesn’t feel the increase in hematocrit is harmful on testosterone...
 forums.t-nation.com
forums.t-nation.com
That makes me the Dummy to continue interacting with someone who won't operate in good faith. Nice chatting again @RobRoy . Can't wait for your next video. Make sure to issue me a public apology. And get Scott on there too.

Benefits of Estrogen for TRT Patients
@readalot I wasn’t going to let you down. Here it is from the smartest man I know. There is some semblance of a chain of reasoning but several aspects are ignored. What does viscosity mean to healthy men without hematological disorders? Do the kinetics of the blood favor developing conditions...
 forums.t-nation.com
forums.t-nation.com
Last edited by a moderator:
Nelson Vergel
Founder, ExcelMale.com
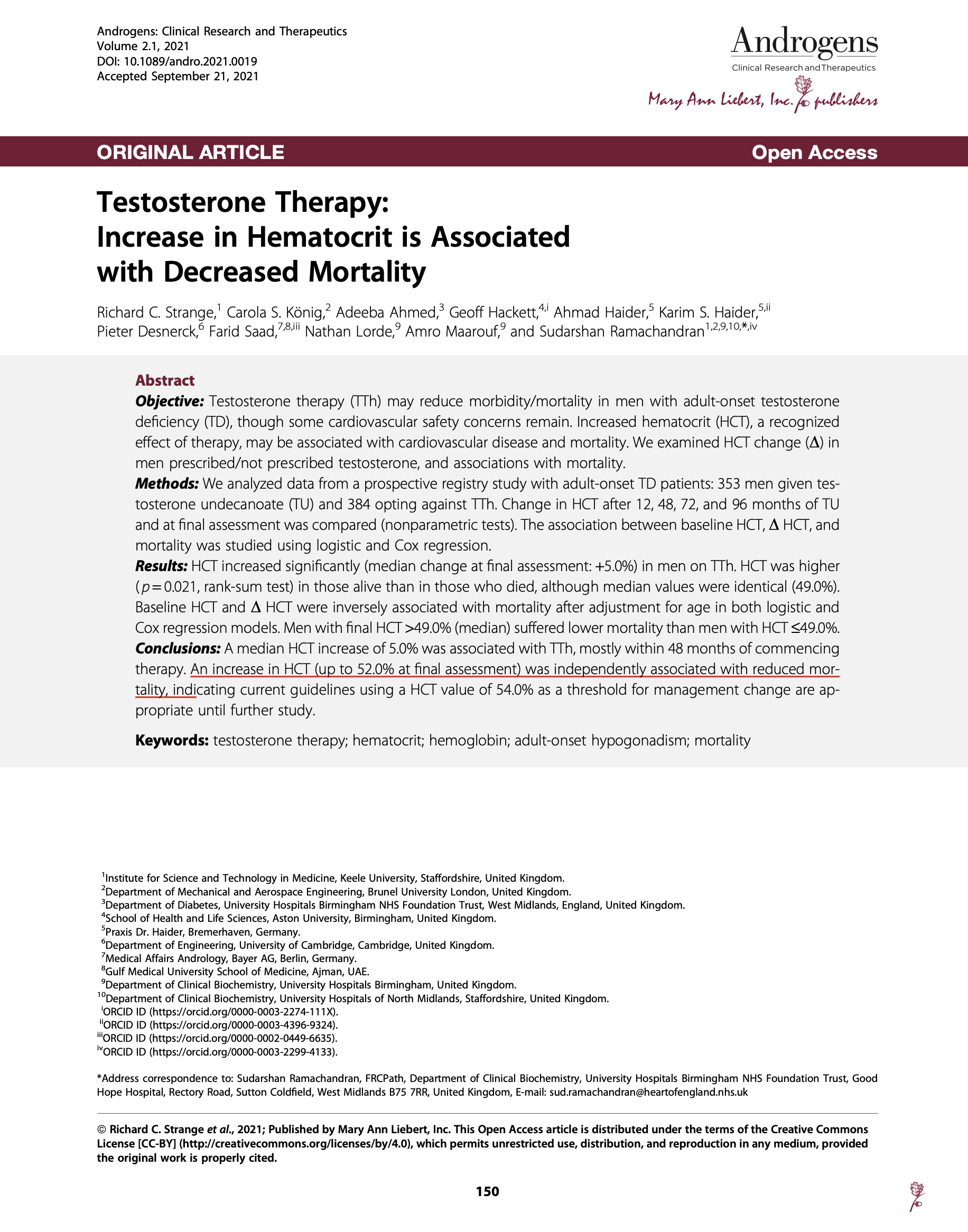
KEY POINTS FROM EMERGING DATA:
TRT for men with low T levels is good for the heart if the hematocrit is not significantly elevated. (Several studies)
TRT for men with low T using T gels: There is no increased heart risk, but there is an increased incidence of palpitations and arrhythmias for some. (TRAVERSE STUDY)
TRT for men on low T who eventually have long term exposure to hematocrit over 52: There is growing evidence that an unmanaged high hematocrit may not be as great, especially during the first year. (Ramasamy)
TRT for men with low T levels is good for the heart if the hematocrit is not significantly elevated. (Several studies)
TRT for men with low T using T gels: There is no increased heart risk, but there is an increased incidence of palpitations and arrhythmias for some. (TRAVERSE STUDY)
TRT for men on low T who eventually have long term exposure to hematocrit over 52: There is growing evidence that an unmanaged high hematocrit may not be as great, especially during the first year. (Ramasamy)
T
tareload
Guest
Also TRT arm showed higher incidence of DVT/PE (tertiary end point). Marginal hazard ratio and read fine print in Table 2. No multiplicity correction for secondary and higher endpoints.TRT for men with low T using T gels: There is no increased heart risk, but there is an increased incidence of palpitations and arrythmias for some. (TRANVERSE STUDY)
Sure looks like reasonable evidence for more clots in the T group. Huge effect size? No. Significant? Likely. Nothing special about using p value of 0.05 to calculate HR. Could use p value of 0.1 or 0.001 or whatever. I will spare everyone a deep dive on statistical significance, means comparisons, p values unless someone really wants it.
This study was about as mild as you can get from invention standpoint. To Nelson's point, an injection study or TOT treatment arm would be illuminating. Evidently I am only person who knows Docs who have had patients throw a clot with TRT, blood pressure, symphathetic NS overdrive, etc. Forget the long term wear and tear as well.. The TOT Knights of the Roundtable and their patients are immune from any T adverse events. Must be nice.
Last edited by a moderator:
Nelson Vergel
Founder, ExcelMale.com
I am showing some interesting patient withdrawal and dropout data here (post #10)

 www.excelmale.com
www.excelmale.com

Effects of Long-term Testosterone Treatment on Cardiovascular Outcomes in Men with Hypogonadism
ABSTRACT Background: Testosterone exerts some effects on the cardiovascular system that could be considered beneficial; some other effects may potentially increase the risk of cardiovascular (CV) events. Neither the long-term efficacy nor safety of testosterone treatment has been studied in an...
Guided_by_Voices
Well-Known Member
" included older men with a high incidence of comorbid conditions.22 While this trial only included 209 men, their demographic information is similar in nature to our study, which included a large proportion of men with comorbid conditions."
In searching for confounders that these studies presumably should have corrected for (e.g. blood pressure, fasting insulin, sun exposure/vitamin D levels, PUFA exposure, visceral fat, CRP, and numerous others) I found nothing, but I did find the above statement that suggests the study was littered with other health issues and unlikely to be representative of people on this forum.
It would also have been interesting to know estrogen levels since estrogen is thought to be somewhat cardio-protective.
For those of us that haven't been following this feud, what are the benefits that those arguing for higher levels cite? As I've posted before, having coached people with frailty issues, if higher T/anabolic levels significantly help resolve that issue, the benefits of that alone would likely outweigh any negatives cited here that can't be mitigated by blood donation and basic harm reduction. As someone who (so far) seems to do better with lower T levels I don't pay too much attention to issues with higher levels, but that could change in the future I suppose.
In searching for confounders that these studies presumably should have corrected for (e.g. blood pressure, fasting insulin, sun exposure/vitamin D levels, PUFA exposure, visceral fat, CRP, and numerous others) I found nothing, but I did find the above statement that suggests the study was littered with other health issues and unlikely to be representative of people on this forum.
It would also have been interesting to know estrogen levels since estrogen is thought to be somewhat cardio-protective.
For those of us that haven't been following this feud, what are the benefits that those arguing for higher levels cite? As I've posted before, having coached people with frailty issues, if higher T/anabolic levels significantly help resolve that issue, the benefits of that alone would likely outweigh any negatives cited here that can't be mitigated by blood donation and basic harm reduction. As someone who (so far) seems to do better with lower T levels I don't pay too much attention to issues with higher levels, but that could change in the future I suppose.
Last edited:
Online statistics
- Members online
- 1
- Guests online
- 8
- Total visitors
- 9
Totals may include hidden visitors.
© Copyright ExcelMale
















