There are valid points on both sides of this.
Fact: polycythemia vera and erythrocytosis are COMPLETELY different phenomena and should not be confused (though the terms are often erroneously used interchangeably). Polycythemia vera is without a doubt MORE risky, but that doesn't mean erythrocytosis comes without (longterm) risk.
Fact: though the physiology is similar, erythrocytosis from TRT is NOT a physiologic erythrocytosis, but is IATROGENIC. Though physiologically similar, the ethics and medico-legal considerations are certainly much different.
Fact: there is no solid data of increased risk of MI, DVT, etc that is attributable directly to appropriate TRT (I know we all agree on this one).
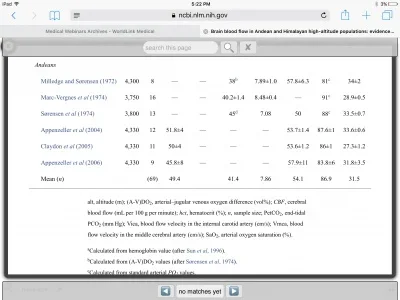
My take: as I've said before, it is not concern for MI, DVT that presents itself to me with TRT-induced erythrocytosis, but more the LONGTERM vascular consequences. To be clear, I'm generally referring to HCT >53 which is about where I draw the line LONGTERM. Most folks at high altitude DO in fact have higher H/H than their counterparts at sea level, however most are NOT HCT > 53 unless they have multiple exacerbating factors contributing (smoker, high iron levels/intake, OSA - this is a BIG one, COPD, + TRT). We all agree higher HCT = more viscous blood. If we look at simple fluid dynamics and the laws of physics, thicker fluid (blood) inside of a pipe (vessel) = higher pressure (blood pressure). I've seen this countless times in patients requiring blood donation or therapeutic phlebotomy -- BP drops, sometimes dramatically, afterwards and generally remains at the lower levels until (if/when) HCT rises again.
Now of course we also have the other end of the equation with enhanced nitric oxide production - which helps as it dilates the pipe (vessel) - consequently counterbalancing the increase in pressure. The problem is that this vasodilation from nitric oxide is VARIABLE over time, whereas the increased HCT is more constant...meaning that this teeter-totter of "thicker blood" counterbalanced by nitric oxide vasodilation, will certainly present times when the viscosity side of the equation is at a distinct advantage. Thinking of it another way, the body is able to adapt REMARKABLY to many differing situations (one of which noted above with the vasodilation), but nonetheless has it's functional limits. Think of it as an airplane that flies at 60-70% of its functional engine capacity (just estimates as I'm not a pilot!) - this piece of machinery has the capacity to utilize a higher percentage of its capacity, but keeping the "normal operating capacity" of the plain at 60-70% gives that added safety margin. The plain can then "throw it into overdrive" and utilize a higher percentage (temporarily) of its capacity when the situation calls for it. This is a crude analogy, but hopefully will make some sense. For the human side - the human body has a capacity to TOLERATE (probably the best term) HCT levels very high under certain situations as an adaptive mechanism, but the higher the HCT goes you are eating into that safety margin for the max capacity of the cardiovascular system and thus reduce the ability of the cardiovascular to remain plastic and adaptable to other changing conditions or insults. For instance, all may be well when the "teeter-totter" of viscosity/nitric oxide is all balanced, but what about when the patient experiences times of reduced nitric oxide production (or other reasons that the pipe won't dilate...like atherosclerosis as they age)...well then the equation is shifted squarely in favor of the higher viscosity = higher BP --> increased shear forces on arterial walls --> increased risk of macro and microvascular pathology, etc.
We don't have longterm data (and likely will not for a long time to come) for MANY of the interesting and debatable talking points related to TRT and other hormonal treatments. We can just weigh the current data we have, use our own clinical judgment and understanding of the physiology of the human body, and sprinkle in a little common sense from time to time to make the decisions we feel are in the best interest of our patients longterm.
I personally would not feel forthright in telling one of my 30-40-50 year old patients that sustaining an iatrogenic erythrocytosis with HCT >53 for the next two, three, or four decades of their life will not present any longterm risk...but it's a debatable topic and one for which each provider (and patient) must determine where they stand and approach it accordingly.