The Vorck Protocol Summary
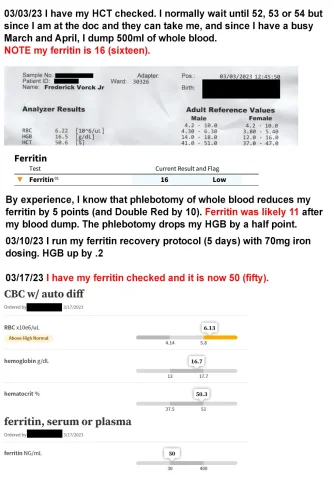
Background: The protocol was developed by a TRT user since 2001 who had difficulty recovering ferritin levels after blood donations. After conducting personal research and consulting with a hematologist in May 2021, he created and tested this protocol on himself and other TRT users with reported success.
The Protocol (Short Version)
Dosage:
- Three 60mg doses of Ferrous bisglycinate chelate per day
- Timing: 9am, 3pm, and 8pm
- Duration: At least 3 consecutive days
Critical Requirements:
- Must NOT take vitamins C and D during the protocol days
- Estradiol levels should ideally be in the 20-60 pg/mL range
- Initial dose must be 60mg or higher
- Do not exceed 300mg total per day
- Precise timing matters
Scientific Rationale
The protocol is based on understanding how hepcidin works in iron metabolism. Rather than simply "blocking absorption" as commonly described, hepcidin actually:
- Binds to and degrades ferroportin
- Traps iron inside cells
- Blocks iron export into serum
- Much of this trapped iron converts to ferritin
Vitamins C and D suppress hepcidin, which increases iron in the blood - something TRT users with high hemoglobin want to avoid.
Reported Results
The creator reported:
- Raised ferritin 10 points in 3 days on first attempt
- Ferritin typically drops 5 points with whole blood donation, 10 points with double red donation
- Recent example: Ferritin at 26, donated 455ml RBCs, followed 4-day protocol, ferritin returned to 28
Hi all, I started TRT in 2001 and have been giving blood over the years and have always had issues with recovering my ferritin. Long story short, I got tired of waiting for others to do the research, so I did it myself, created a protocol, hired a hematologist in May 2021 who thought it could work, ran it by him, and tried it on myself. It worked (I was able on my first try to raise ferritin 10 points in 3 days, but I've learned more since then). I have shared it with other guys on TRT who have seen the same success. Now I'd like to share it with you.
How to raise ferritin, the short version
Three 60mg doses a day of Ferrous bisglycinate chelate spaced apart at 9am, 3pm, and 8pm all on the same day, at least 3 days in a row. You MUST NOT be taking vitamins C and D. Your Estradiol should ideally be 20-60pg/mL range. (I'm not saying never take vitamins C and D. Just not during these days.) The times of day absolutely do matter. Your initial dose of iron MUST be 60mg or higher. Subsequent doses may be 60 or higher. Right now I'm telling people do not exceed 300mg in a day.
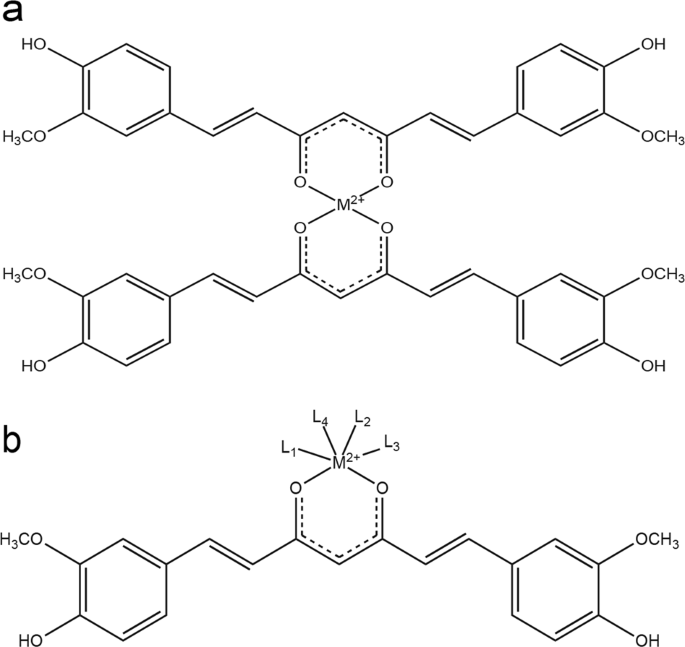
The key to raising ferritin is understanding how hepcidin works. Saying that it "blocks absorption" as you see in a lot of blogs is incredibly misleading. It binds to and degrades ferroportin, trapping iron in cells and blocking export of iron into serum. A large portion of that trapped iron will become ferritin. Vitamins C and D both crush hepcidin (which obviously increases the amount of iron in your blood, but guys with high hemoglobin want to avoid that).
My ferritin drops 5 points with a donation of whole and 10 points with a double red donation. Most recently, my ferritin was at 26. I donated 455ml of RBCs, followed my post-donation protocol for 4 days, and my ferritin was at 28. My intention is to develop my protocol further with more days and use of Adenine. The point for now is that you can put ferritin back to where it was pre-donation.
I have this written up in lengthier form because it's a LOT, and I wanted to explain everything about it to doubters and put sources to it. I have the long explanation here on my own, non-commercial site:
Last edited by a moderator: