madman
Super Moderator
Management of Erythrocytosis in Men Receiving Testosterone Therapy: Clinical Consultation Guide (2022)
Pranjal Agrawal, Sajya M. Singh, Taylor Kohn
1. Introduction
Testosterone deficiency, previously known as male hypogonadism, affects approximately 25% of all men, with a prevalence that increases with age [1]. Risk factors for developing adult-onset testosterone deficiency include obesity, chronic disease, and poor general health [2]. Individuals with clinical hypogonadal symptoms and two-morning samples demonstrating low testosterone levels often benefit from testosterone therapy (TT).
The European Association of Urology (EAU) lists the following as primary indications for TT: delayed puberty; Klinefelter’s syndrome with hypogonadism; sexual dysfunction, including erectile dysfunction not responding to phosphodiesterase-5 inhibitors (PDE5i); osteoporosis due to hypogonadism; hypopituitarism; and adult men with testosterone levels lower than an age-specific physiological range exhibiting hypogonadal symptoms [3,4]. The primary aim of TT is to reduce clinical symptoms of testosterone deficiency by restoring serum testosterone levels to an age-dependent mid-normal range [3,4].
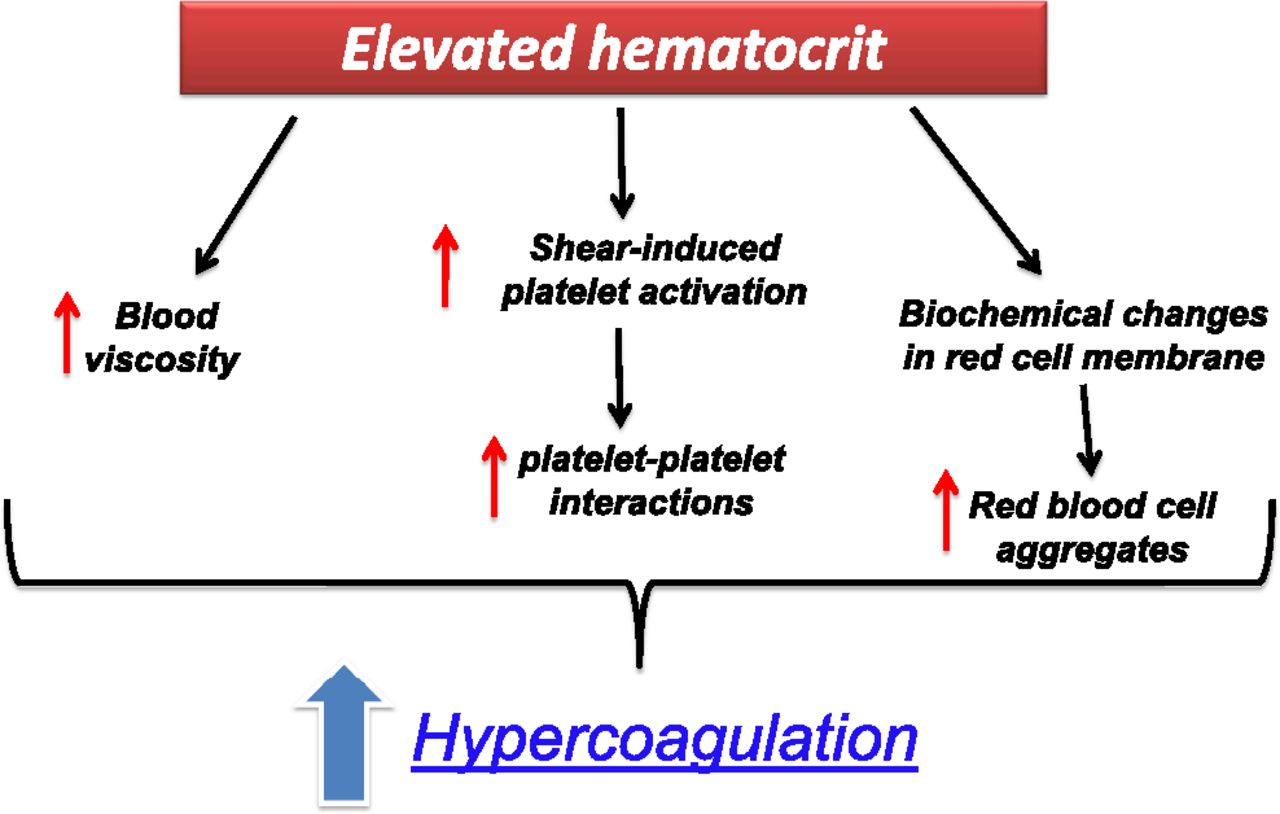
However, TT can lead to adverse effects, including, most commonly, erythrocytosis or an increase in hemoglobin (Hb) and hematocrit (Hct) levels [3,4]. A recent study demonstrated that erythrocytosis in men on TT is an independent risk factor for major adverse cardiovascular events (MACE) and venous thromboembolism (VTE) within the first year of treatment onset [5]. In fact, the EAU lists Hct >54% as a contraindication for TT [3,4]. Low testosterone levels have been associated with an unfavorable prognosis for prostate cancer, although this association is still a matter of debate [6]. Therefore, the benefits of TT must be weighed against the higher cardiovascular risk associated with the initiation of therapy. Furthermore, any development of erythrocytosis while on TT must be promptly identified and managed.
2. Does the TT route, duration, or dosage matter?
3. Management of erythrocytosis
4. Conclusions
Erythrocytosis is the most common side effect of all TT modalities. Patient-specific factors should be considered when choosing an appropriate TT dosage and modality. Owing to the risk of MACE and VTE, Hct >54% should prompt providers to consider decreasing and discontinuing TT until normalization of Hct.
Pranjal Agrawal, Sajya M. Singh, Taylor Kohn
1. Introduction
Testosterone deficiency, previously known as male hypogonadism, affects approximately 25% of all men, with a prevalence that increases with age [1]. Risk factors for developing adult-onset testosterone deficiency include obesity, chronic disease, and poor general health [2]. Individuals with clinical hypogonadal symptoms and two-morning samples demonstrating low testosterone levels often benefit from testosterone therapy (TT).
The European Association of Urology (EAU) lists the following as primary indications for TT: delayed puberty; Klinefelter’s syndrome with hypogonadism; sexual dysfunction, including erectile dysfunction not responding to phosphodiesterase-5 inhibitors (PDE5i); osteoporosis due to hypogonadism; hypopituitarism; and adult men with testosterone levels lower than an age-specific physiological range exhibiting hypogonadal symptoms [3,4]. The primary aim of TT is to reduce clinical symptoms of testosterone deficiency by restoring serum testosterone levels to an age-dependent mid-normal range [3,4].
However, TT can lead to adverse effects, including, most commonly, erythrocytosis or an increase in hemoglobin (Hb) and hematocrit (Hct) levels [3,4]. A recent study demonstrated that erythrocytosis in men on TT is an independent risk factor for major adverse cardiovascular events (MACE) and venous thromboembolism (VTE) within the first year of treatment onset [5]. In fact, the EAU lists Hct >54% as a contraindication for TT [3,4]. Low testosterone levels have been associated with an unfavorable prognosis for prostate cancer, although this association is still a matter of debate [6]. Therefore, the benefits of TT must be weighed against the higher cardiovascular risk associated with the initiation of therapy. Furthermore, any development of erythrocytosis while on TT must be promptly identified and managed.
2. Does the TT route, duration, or dosage matter?
3. Management of erythrocytosis
4. Conclusions
Erythrocytosis is the most common side effect of all TT modalities. Patient-specific factors should be considered when choosing an appropriate TT dosage and modality. Owing to the risk of MACE and VTE, Hct >54% should prompt providers to consider decreasing and discontinuing TT until normalization of Hct.

















