Here is how I use ChatGPT to interpret medical tests.
View attachment 50315
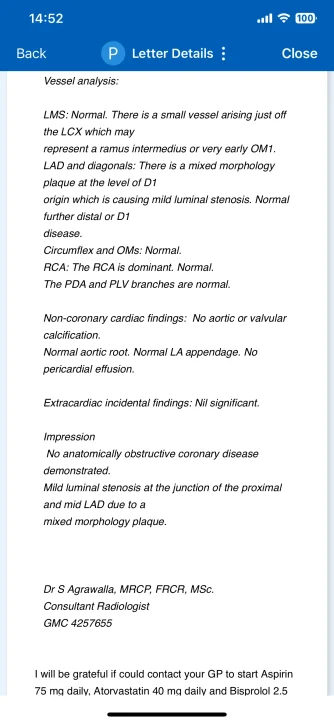
Below is a plain-language explanation of what the report is saying, section by section. Please remember that this interpretation is for general educational purposes and does not replace individualized medical advice from your own doctor.
1.
- LMS (Left Main Stem): This is the main vessel branching off from the aorta to supply blood to the left side of the heart. The report says your LMS is normal with no significant narrowing or blockage.
- LCX (Left Circumflex) and OM (Obtuse Marginal) branches: These vessels supply blood to a portion of the left side of the heart (the side and back). They appear normal on your scan.
- RCA (Right Coronary Artery): This artery typically supplies blood to the right side of the heart and the back part of the left ventricle. The report indicates the RCA is dominant (which is common) and normal, with its branches (PDA and PLV) also described as normal.
2.
- LAD (Left Anterior Descending) and Diagonal Branch:
- The LAD supplies blood to the front part of the heart and is one of the most important arteries. The scan found a “mixed morphology plaque” at the origin of a diagonal branch (D1).
- This plaque is causing mild luminal stenosis—that is, a mild narrowing of the artery’s inner channel. The fact that it's called “mixed morphology” means the plaque likely contains different tissue types (for example, areas of calcium along with softer fatty material).
- Beyond that small area of mild narrowing, the rest of the LAD and its diagonal branches were reported as normal.
3.
- No Aortic or Heart Valve Calcification: This means your main vessel leaving the heart (the aorta) and the valves inside your heart do not show significant calcium buildup.
- Normal Aortic Root, LA (Left Atrial) Appendage: These structures appear typical in size and shape.
- No Pericardial Effusion: There’s no excess fluid in the sac surrounding your heart.
4.
- “No anatomically obstructive coronary disease demonstrated”: This means you do not have a severe blockage (nothing at or above the levels usually considered dangerous, such as 70% narrowing or more).
- “Mild luminal stenosis” in one spot in the LAD: This is a relatively small narrowing. Your doctor may still consider it important to manage risk factors to prevent progression.
5.
- Aspirin (low dose): Helps reduce the likelihood of blood clots forming on any plaque.
- Atorvastatin (a cholesterol-lowering medication): Helps stabilize and possibly reduce plaque in the arteries over time, plus lowers LDL (“bad cholesterol”).
- Bisoprolol (a beta-blocker): Helps manage blood pressure, heart rate, and overall cardiac workload, which can protect the heart and slow plaque progression.
6.
- Your main arteries look good overall: There is no major blockage that severely compromises blood flow.
- You have one area of mild narrowing in an important artery (the LAD), but it’s not severe.
- Preventive measures—like medications to lower cholesterol, reduce clot formation, and control blood pressure/heart rate—are recommended to maintain heart health, keep plaque in check, and lower future cardiovascular risk.
- Lifestyle habits—such as maintaining a healthy diet, exercising regularly, and avoiding smoking—play a big role in preventing progression of any plaque.
7.
- Follow-Up with Your Doctor: They may want periodic checkups or further tests (such as stress tests or follow-up imaging) to monitor that mild plaque.
- Manage Risk Factors: Keep an eye on cholesterol levels, blood pressure, blood sugar (if relevant), and maintain healthy habits like balanced nutrition and regular physical activity.
- Take Medications as Prescribed: These help prevent further buildup and reduce the risk of heart events.
Bottom Line: Your heart arteries are in generally good shape, with only a mild narrowing detected. By sticking to the recommended medications and healthy lifestyle measures, you’ll give yourself the best chance of keeping your arteries clear and preventing any future heart issues. Always discuss specific concerns and treatment questions with your cardiologist or primary care physician.