I have an LAD stent after angina with exertion at age 54, no MI, 95-98% occlusion.
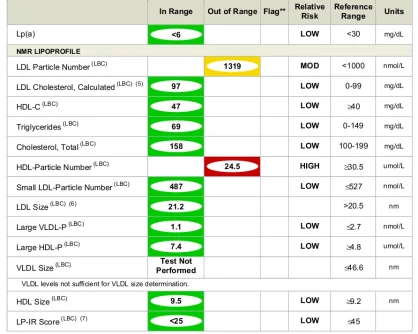
LPa 6, ref range <30mg/dl
No other significant risks in Cleveland Heart labs/lipidology, Previous heart scan showed tiny-minimal calcification way downstream in a R side artery, not considered a risk.
Not overweight, active, no diabetic troubles or insulin resistance, etc.
Only ongoing marker not ideal, low-ish HDL
Shit happens regardless of your numbers.
Did the 95-98% occlusion show up on the previous heart scan?