Nelson Vergel
Founder, ExcelMale.com
This is probably the best relatively short medical review of male infertility I have read in a long time. A must read for those of you who are having issues in that area.
Quotes:
About 15% of couples have difficulty conceiving, and in approximately 30% of these couples only the man has reproductive dysfunction. In another 20% of the subfertile couples, both partners have a reproductive abnormality. Thus, male reproductive dysfunction contributes to about half of all cases of subfertile couples.
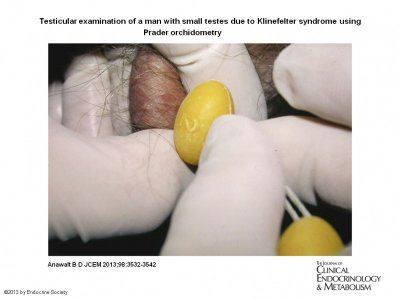
....More commonly, gonadotropin replacement therapy is generally administered as LH and FSH replacement therapy. After any exogenous androgen therapy has been discontinued, LH replacement therapy is initiated as human chorionic gonadotropin (hCG). The usual dosage of hCG is 1000–2000 IU sc 2–3 times weekly, but it is likely that lower dosages of 500–750 IU are effective (30, 31). Because some men (particularly men with pretreatment testes ≥ 8 cc) will produce sperm and become fertile with hCG alone, and because FSH therapy is expensive, hCG is often administered as monotherapy for 6 months, whereas sperm concentrations are measured monthly. If the patient can afford early initiation of FSH therapy, it could be initiated immediately and might result in more rapid increases in sperm concentrations. Men with postpubertal gonadotropin deficiency might respond to hCG monotherapy, but men with prepubertal onset of gonadotropin deficiency virtually always benefit from combination hCG plus FSH therapy. Sperm concentrations typically take at least 4–6 months to rise with hCG monotherapy, and FSH therapy is added if sperm concentrations remain below 10 million/mL and conception has not occurred. FSH may be given as recombinant human FSH (rhFSH) or human menopausal gonadotropin; the usual initial dosage is 75 IU sc every other day. The dosage of FSH may be doubled if conception has not occurred and sperm concentrations remain < 20 million/mL within 6 months of initiation of combination therapy with hCG. On average, conception occurs after 2–3 years of gonadotropin therapy and occurs when sperm concentrations are between 5 and 20 million/mL, but conception may occur at levels (<5 million/mL) well below the levels (13–20 million/mL) associated with fertility in normal men (32). If the couple desires another child within 2 years, then gonadotropin therapy should be continued until another pregnancy is achieved.Men with baseline small testes ≤ 4 cc are more likely to respond slowly (33). There is some controversy over whether prior androgen therapy may decrease the likelihood of response to gonadotropin therapy, but the author believes that this effect is unlikely or small at worst (32).
http://jcem.endojournals.org/content/98/9/3532.full
Quotes:
About 15% of couples have difficulty conceiving, and in approximately 30% of these couples only the man has reproductive dysfunction. In another 20% of the subfertile couples, both partners have a reproductive abnormality. Thus, male reproductive dysfunction contributes to about half of all cases of subfertile couples.
....More commonly, gonadotropin replacement therapy is generally administered as LH and FSH replacement therapy. After any exogenous androgen therapy has been discontinued, LH replacement therapy is initiated as human chorionic gonadotropin (hCG). The usual dosage of hCG is 1000–2000 IU sc 2–3 times weekly, but it is likely that lower dosages of 500–750 IU are effective (30, 31). Because some men (particularly men with pretreatment testes ≥ 8 cc) will produce sperm and become fertile with hCG alone, and because FSH therapy is expensive, hCG is often administered as monotherapy for 6 months, whereas sperm concentrations are measured monthly. If the patient can afford early initiation of FSH therapy, it could be initiated immediately and might result in more rapid increases in sperm concentrations. Men with postpubertal gonadotropin deficiency might respond to hCG monotherapy, but men with prepubertal onset of gonadotropin deficiency virtually always benefit from combination hCG plus FSH therapy. Sperm concentrations typically take at least 4–6 months to rise with hCG monotherapy, and FSH therapy is added if sperm concentrations remain below 10 million/mL and conception has not occurred. FSH may be given as recombinant human FSH (rhFSH) or human menopausal gonadotropin; the usual initial dosage is 75 IU sc every other day. The dosage of FSH may be doubled if conception has not occurred and sperm concentrations remain < 20 million/mL within 6 months of initiation of combination therapy with hCG. On average, conception occurs after 2–3 years of gonadotropin therapy and occurs when sperm concentrations are between 5 and 20 million/mL, but conception may occur at levels (<5 million/mL) well below the levels (13–20 million/mL) associated with fertility in normal men (32). If the couple desires another child within 2 years, then gonadotropin therapy should be continued until another pregnancy is achieved.Men with baseline small testes ≤ 4 cc are more likely to respond slowly (33). There is some controversy over whether prior androgen therapy may decrease the likelihood of response to gonadotropin therapy, but the author believes that this effect is unlikely or small at worst (32).
http://jcem.endojournals.org/content/98/9/3532.full