T
tareload
Guest
Hi ExcelMale folks, I wanted to start off by expressing my gratitude for this site, all of the amazing work that has been put in to make this place such a great source of information. I would expect no less from a chemical engineer  .
.
I've been following this "debate" about how to properly manage TRT users and hematocrit levels and am really shocked. I'm not going to link to the videos or podcasts that have surfaced recently in this post directly but the debates corresponding to this concept have been covered here at ExcelMale.
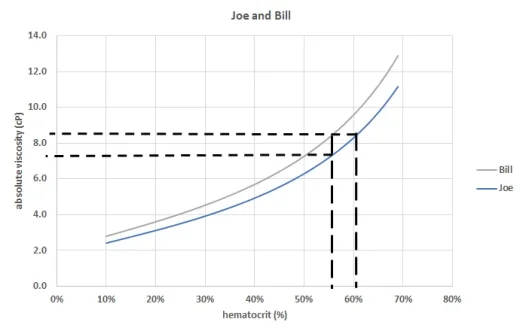
I actually listened to a recent podcast where the host suggested a Hct level of 55% is optimal, but didn't fully disclose what the objective function was. It's an important clarification: longevity/performance/what? What worries me about the recommendations I've listened to is that some poor fellow is going to use this advice and think an Hct level in the mid 50s is perfectly reasonable and nothing should be done to correct this. Again, depending on this person's objective function (i.e., a competitive athlete) maybe they shouldn't do anything in the short term to maximize athletic performance. But for the vast majority of folks looking for functional longevity and compression of morbidity, the medical literature is quite clear a corrective action should be taken. In this thread I'll share some literature, resources to help inform TRT users and demonstrate that elevated Hct is not benign.
I can't think of a better way to think about this topic that what Dr. Saya states many times that it's about "balance" as you are trying to juggle a host of feedback loops and physiological responses. Don't screw yourself up and think that long term elevation of hematocrit is no big deal. I hope you enjoy the reading material so you can make an informed decision about your health. You are taking a healthy step forward to correct hormonal deficiency so don't then take a step back when it comes to your heart and ignoring elevated Hct.
Here's a recent review article that discusses the vascular remodeling response to increased blood viscosity. The first question you should ask yourself before reading this is: if increased blood viscosity is of no concern then why have mammals evolved to possess this response? More to come...
The systemic vascular resistance response: a cardiovascular response modulating blood viscosity with implications for primary hypertension and certain anemias
I've been following this "debate" about how to properly manage TRT users and hematocrit levels and am really shocked. I'm not going to link to the videos or podcasts that have surfaced recently in this post directly but the debates corresponding to this concept have been covered here at ExcelMale.
The community at ExcelMale is very fortunate to have Nelson (a chemical engineer who understand fluid dynamics) and Dr. Saya who has a remarkable mind. His discussion in the above link is spot on.I actually listened to a recent podcast where the host suggested a Hct level of 55% is optimal, but didn't fully disclose what the objective function was. It's an important clarification: longevity/performance/what? What worries me about the recommendations I've listened to is that some poor fellow is going to use this advice and think an Hct level in the mid 50s is perfectly reasonable and nothing should be done to correct this. Again, depending on this person's objective function (i.e., a competitive athlete) maybe they shouldn't do anything in the short term to maximize athletic performance. But for the vast majority of folks looking for functional longevity and compression of morbidity, the medical literature is quite clear a corrective action should be taken. In this thread I'll share some literature, resources to help inform TRT users and demonstrate that elevated Hct is not benign.
I can't think of a better way to think about this topic that what Dr. Saya states many times that it's about "balance" as you are trying to juggle a host of feedback loops and physiological responses. Don't screw yourself up and think that long term elevation of hematocrit is no big deal. I hope you enjoy the reading material so you can make an informed decision about your health. You are taking a healthy step forward to correct hormonal deficiency so don't then take a step back when it comes to your heart and ignoring elevated Hct.
Here's a recent review article that discusses the vascular remodeling response to increased blood viscosity. The first question you should ask yourself before reading this is: if increased blood viscosity is of no concern then why have mammals evolved to possess this response? More to come...
The systemic vascular resistance response: a cardiovascular response modulating blood viscosity with implications for primary hypertension and certain anemias
The systemic vascular resistance response: a cardiovascular response modulating blood viscosity with implications for primary hypertension and certain anemias
Gregory D. Sloop, Joseph J. Weidman, John A. St. Cyr
First Published June 25, 2015 Review Article
https://doi.org/10.1177/1753944715591450
Abstract
Without an active regulatory feedback loop, increased blood viscosity could lead to a vicious cycle of ischemia, increased erythropoiesis, further increases of blood viscosity, decreased tissue perfusion with worsened ischemia, further increases in red cell mass, etc. We suggest that an increase in blood viscosity is detected by mechanoreceptors in the left ventricle which upregulate expression of cardiac natriuretic peptides and soluble erythropoietin receptor. This response normalizes systemic vascular resistance and blood viscosity at the cost of producing ‘anemia of chronic disease or inflammation’ or ‘hemolytic anemia’ both of which are better described as states of compensated hyperviscosity. Besides its role in disease, this response is also active in the physiologic adaptation to chronic exercise. Malfunction of this response may cause primary hypertension.
Last edited by a moderator: