From:
[email protected]

"I am excited to share the results of my study...Women with Thyroid Disease: Treatment Experiences and theDoctor-Patient Relationship. Many months ago, 16 of you participated in my study...thank you SO much. I am currently working to get this study published in the scholarly literature. I hope to get my study into the hands of doctors who can learn from us...I couldn't have done this without you! Together, I believe we can make a difference."
Introduction
Approximately 200 million people worldwide have been diagnosed with thyroid disease, a chronic illness (Rajoria et al., 2010). According to the American Association of Clinical Endocrinologists (AACE, 2013), approximately 30 million Americans are affected by thyroid disease, although more than half remain undiagnosed. Across cultures, the prevalence of thyroid disease is much higher among women than among men (Canaris, Manowitz, Mayor, & Ridgway, 2000; Cassidy, Ahearn, & Carroll, 2002). In fact, women have an estimated 1 in 7 chance of developing thyroid disease (Godfrey, 2007).
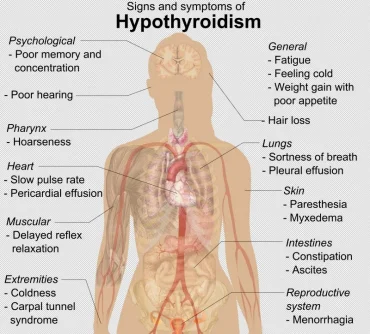
A number of factors make proper diagnosis and treatment of thyroid disease challenging. For example, according to Adams (2008) and Dayan (2001), the most commonly used blood test (thyroid stimulating hormone [TSH]) for diagnosing thyroid disease can produce misleading results. More specifically, although use of all three main thyroid function tests (TSH, free T3, free T4) produces the most thorough analysis of thyroid function, the TSH test tends to be used alone (Dayan, 2001). Because of this, clinically important diagnoses (e.g., hyperthyroidism, hypothyroidism) are sometimes missed. In addition, as thyroid dysfunction produces symptoms similar to those of other disorders (e.g., depression, menopause), thyroid disease is often misdiagnosed and left untreated (Canaris et al., 2000; Godfrey, 2007; Simmons, 2010). Likewise, as the TSH test tends to be used alone to determine treatment effectiveness, many women with thyroid disease continue to experience symptoms even when they are receiving treatment (Bunevicius & Prange, 2006). In the face of such challenges, a doctor-patient relationship based on mutual trust and collaboration helps to ensure positive treatment outcomes (Houle, Harwood, Watkins, & Baum, 2007; Munch, 2004). In addition, effective communication between doctors and patients is critical in both the diagnosis and management of thyroid disease (Shimabukuro, 2008; Simmons, 2010). However, the culture of the medical profession, diagnostic bias, and gender differences in communication may interfere with doctor-patient discourse (Cheney & Ashcraft, 2007; Hamberg, Risberg, & Johansson, 2004; Hoffmann & Tarzian, 2001; Kaiser, 2002; Munch, 2004).
An exploration of women's experiences in the treatment of thyroid disease, especially relative to these three points, may contribute to better understanding on the part of doctors and thus more effective doctor-patient communication and relationships.
Despite the pervasiveness of thyroid disease in women and the importance of the doctor-patient relationship in positive treatment outcomes, there is a gap in the literature regarding the treatment experiences of women diagnosed with thyroid disease, particularly regarding the doctor-patient relationship. Therefore, the purpose of this study was to explore female thyroid patients' experiences of treatment and the doctor-patient relationship.
The following issues were addressed in regard to their relationship with women's treatment experiences: (a) the culture of the medical profession (see Kaiser, 2002; Thomas, 2001), (b) diagnostic bias (see Hamberg et al., 2004; Hoffmann & Tarzian, 2001; Munch, 2004), and (c) gender differences in communication (see Cheney & Ashcraft, 2007; Tannen, 2007).
More information attached.
[email protected]
"I am excited to share the results of my study...Women with Thyroid Disease: Treatment Experiences and theDoctor-Patient Relationship. Many months ago, 16 of you participated in my study...thank you SO much. I am currently working to get this study published in the scholarly literature. I hope to get my study into the hands of doctors who can learn from us...I couldn't have done this without you! Together, I believe we can make a difference."
Introduction
Approximately 200 million people worldwide have been diagnosed with thyroid disease, a chronic illness (Rajoria et al., 2010). According to the American Association of Clinical Endocrinologists (AACE, 2013), approximately 30 million Americans are affected by thyroid disease, although more than half remain undiagnosed. Across cultures, the prevalence of thyroid disease is much higher among women than among men (Canaris, Manowitz, Mayor, & Ridgway, 2000; Cassidy, Ahearn, & Carroll, 2002). In fact, women have an estimated 1 in 7 chance of developing thyroid disease (Godfrey, 2007).
A number of factors make proper diagnosis and treatment of thyroid disease challenging. For example, according to Adams (2008) and Dayan (2001), the most commonly used blood test (thyroid stimulating hormone [TSH]) for diagnosing thyroid disease can produce misleading results. More specifically, although use of all three main thyroid function tests (TSH, free T3, free T4) produces the most thorough analysis of thyroid function, the TSH test tends to be used alone (Dayan, 2001). Because of this, clinically important diagnoses (e.g., hyperthyroidism, hypothyroidism) are sometimes missed. In addition, as thyroid dysfunction produces symptoms similar to those of other disorders (e.g., depression, menopause), thyroid disease is often misdiagnosed and left untreated (Canaris et al., 2000; Godfrey, 2007; Simmons, 2010). Likewise, as the TSH test tends to be used alone to determine treatment effectiveness, many women with thyroid disease continue to experience symptoms even when they are receiving treatment (Bunevicius & Prange, 2006). In the face of such challenges, a doctor-patient relationship based on mutual trust and collaboration helps to ensure positive treatment outcomes (Houle, Harwood, Watkins, & Baum, 2007; Munch, 2004). In addition, effective communication between doctors and patients is critical in both the diagnosis and management of thyroid disease (Shimabukuro, 2008; Simmons, 2010). However, the culture of the medical profession, diagnostic bias, and gender differences in communication may interfere with doctor-patient discourse (Cheney & Ashcraft, 2007; Hamberg, Risberg, & Johansson, 2004; Hoffmann & Tarzian, 2001; Kaiser, 2002; Munch, 2004).
An exploration of women's experiences in the treatment of thyroid disease, especially relative to these three points, may contribute to better understanding on the part of doctors and thus more effective doctor-patient communication and relationships.
Despite the pervasiveness of thyroid disease in women and the importance of the doctor-patient relationship in positive treatment outcomes, there is a gap in the literature regarding the treatment experiences of women diagnosed with thyroid disease, particularly regarding the doctor-patient relationship. Therefore, the purpose of this study was to explore female thyroid patients' experiences of treatment and the doctor-patient relationship.
The following issues were addressed in regard to their relationship with women's treatment experiences: (a) the culture of the medical profession (see Kaiser, 2002; Thomas, 2001), (b) diagnostic bias (see Hamberg et al., 2004; Hoffmann & Tarzian, 2001; Munch, 2004), and (c) gender differences in communication (see Cheney & Ashcraft, 2007; Tannen, 2007).
More information attached.
Attachments
Last edited by a moderator:














