Nelson Vergel
Founder, ExcelMale.com
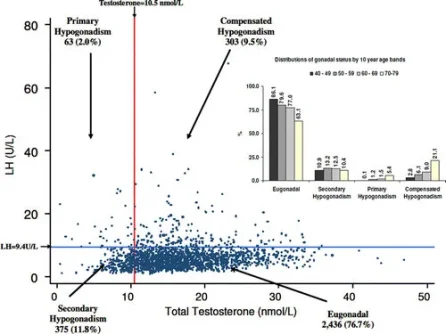
A man with compensated hypogonadism may have high LH with normal total testosterone blood levels.
In previous studies, a significant proportion of older men have been shown to have high gonadotropins and T within the normal range. This raises the possibility of a state of compensated, or subclinical, hypogonadism that may eventually develop into overt primary hypogonadism. An analogous situation is well recognized in the pituitary-thyroid axis where high TSH, in the face of normal thyroid hormone levels, is the hallmark of subclinical hypothyroidism.
In this study, we investigated whether specific risk factors or clinical features can differentiate between secondary, primary, and the new putative form of compensated hypogonadism categorized biochemically in participants from the European Male Ageing Study (EMAS), a community-based study of middle-aged and elderly men.
http://press.endocrine.org/doi/full/10.1210/jc.2009-1796

Characteristics of Compensated Hypogonadism in Patients with Sexual Dysfunction
Corona G, Maseroli E, Rastrelli G, et al. Characteristics of Compensated Hypogonadism in Patients with Sexual Dysfunction. The Journal of Sexual Medicine. http://onlinelibrary.wiley.com/doi/10.1111/jsm.12549/abstract
Introduction
In the last few years, a view that subclinical endocrine disorders represent milder forms of the clinically overt disease has emerged. Accordingly, it has been proposed that compensated hypogonadism represents a genuine clinical subset of late-onset hypogonadism.
Aim
The aim of the present study is to investigate the associations of compensated hypogonadism with particular clinical and psychological characteristics of male subjects complaining of sexual dysfunction.
Methods
After excluding documented genetic causes of hypogonadism, an unselected consecutive series of 4,173 patients consulting our unit for sexual dysfunction was studied. Compensated hypogonadism was identified according to the European Male Ageing study criteria: total testosterone ≥10.5 nmol/L and luteinizing hormone >9.4 U/L.
Main Outcome Measures
Several hormonal, biochemical, and instrumental (penile Doppler ultrasound) parameters were studied, along with results of the Structured Interview on Erectile Dysfunction (SIEDY) and ANDROTEST.
Results
One hundred seventy (4.1%) subjects had compensated hypogonadism, whereas 827 (19.8%) had overt hypogonadism. After adjustment for confounding factors, no specific sexual symptoms were associated with compensated hypogonadism. However, compensated hypogonadism individuals more often reported psychiatric symptoms, as detected by Middlesex Hospital Questionnaire score, when compared with both eugonadal and overt hypogonadal subjects (adjusted odds ratios = 1.018 [1.005;1.031] and 1.014 [1.001;1.028], respectively; both P < 0.005). In addition, subjects with compensated or overt hypogonadism had an increased predicted risk of cardiovascular events (as assessed by Progetto Cuore risk algorithm) when compared with eugonadal individuals. Accordingly, mortality related to major adverse cardiovascular events (MACEs), but not MACE incidence, was significantly higher in subjects with both compensated and overt hypogonadism when compared with eugonadal subjects.
Conclusions
The present data do not support the concept that compensated (subclinical) hypogonadism represents a new clinical entity. The possibility that subclinical hypogonadism could be a normal response of the hypothalamus–pituitary–testis axis to somatic illness should be considered. Further studies are urgently needed to clarify this latter point.
In previous studies, a significant proportion of older men have been shown to have high gonadotropins and T within the normal range. This raises the possibility of a state of compensated, or subclinical, hypogonadism that may eventually develop into overt primary hypogonadism. An analogous situation is well recognized in the pituitary-thyroid axis where high TSH, in the face of normal thyroid hormone levels, is the hallmark of subclinical hypothyroidism.
In this study, we investigated whether specific risk factors or clinical features can differentiate between secondary, primary, and the new putative form of compensated hypogonadism categorized biochemically in participants from the European Male Ageing Study (EMAS), a community-based study of middle-aged and elderly men.
http://press.endocrine.org/doi/full/10.1210/jc.2009-1796
Characteristics of Compensated Hypogonadism in Patients with Sexual Dysfunction
Corona G, Maseroli E, Rastrelli G, et al. Characteristics of Compensated Hypogonadism in Patients with Sexual Dysfunction. The Journal of Sexual Medicine. http://onlinelibrary.wiley.com/doi/10.1111/jsm.12549/abstract
Introduction
In the last few years, a view that subclinical endocrine disorders represent milder forms of the clinically overt disease has emerged. Accordingly, it has been proposed that compensated hypogonadism represents a genuine clinical subset of late-onset hypogonadism.
Aim
The aim of the present study is to investigate the associations of compensated hypogonadism with particular clinical and psychological characteristics of male subjects complaining of sexual dysfunction.
Methods
After excluding documented genetic causes of hypogonadism, an unselected consecutive series of 4,173 patients consulting our unit for sexual dysfunction was studied. Compensated hypogonadism was identified according to the European Male Ageing study criteria: total testosterone ≥10.5 nmol/L and luteinizing hormone >9.4 U/L.
Main Outcome Measures
Several hormonal, biochemical, and instrumental (penile Doppler ultrasound) parameters were studied, along with results of the Structured Interview on Erectile Dysfunction (SIEDY) and ANDROTEST.
Results
One hundred seventy (4.1%) subjects had compensated hypogonadism, whereas 827 (19.8%) had overt hypogonadism. After adjustment for confounding factors, no specific sexual symptoms were associated with compensated hypogonadism. However, compensated hypogonadism individuals more often reported psychiatric symptoms, as detected by Middlesex Hospital Questionnaire score, when compared with both eugonadal and overt hypogonadal subjects (adjusted odds ratios = 1.018 [1.005;1.031] and 1.014 [1.001;1.028], respectively; both P < 0.005). In addition, subjects with compensated or overt hypogonadism had an increased predicted risk of cardiovascular events (as assessed by Progetto Cuore risk algorithm) when compared with eugonadal individuals. Accordingly, mortality related to major adverse cardiovascular events (MACEs), but not MACE incidence, was significantly higher in subjects with both compensated and overt hypogonadism when compared with eugonadal subjects.
Conclusions
The present data do not support the concept that compensated (subclinical) hypogonadism represents a new clinical entity. The possibility that subclinical hypogonadism could be a normal response of the hypothalamus–pituitary–testis axis to somatic illness should be considered. Further studies are urgently needed to clarify this latter point.











