You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
My CAC calcium score is high- Should I take vitamin K?
- Thread starter Ronnny
- Start date
-
- Tags
- artery calcium score heart plaque
Nelson Vergel
Founder, ExcelMale.com
Vince
Super Moderator
Get a real cholesterol panel that's a good way to start slowing your growth of plaque. If you keep your growth to 10% or less your arteries will adjust and you will never have a heart attack or stroke.

 www.excelmale.com
www.excelmale.com

Cleveland Heart Clinic Labs
I was just wondering if anyone uses Cleveland Heart Labs http://www.knowyourrisk.com/ My clinic http://advlip.com/ will now be using them for all Labs. Will also check my LDL oxidation. CHL is a spinoff of Cleveland Clinic, I know they do all the advanced tests and I believe they actually...
Nelson Vergel
Founder, ExcelMale.com
This is a detailed lipid panel
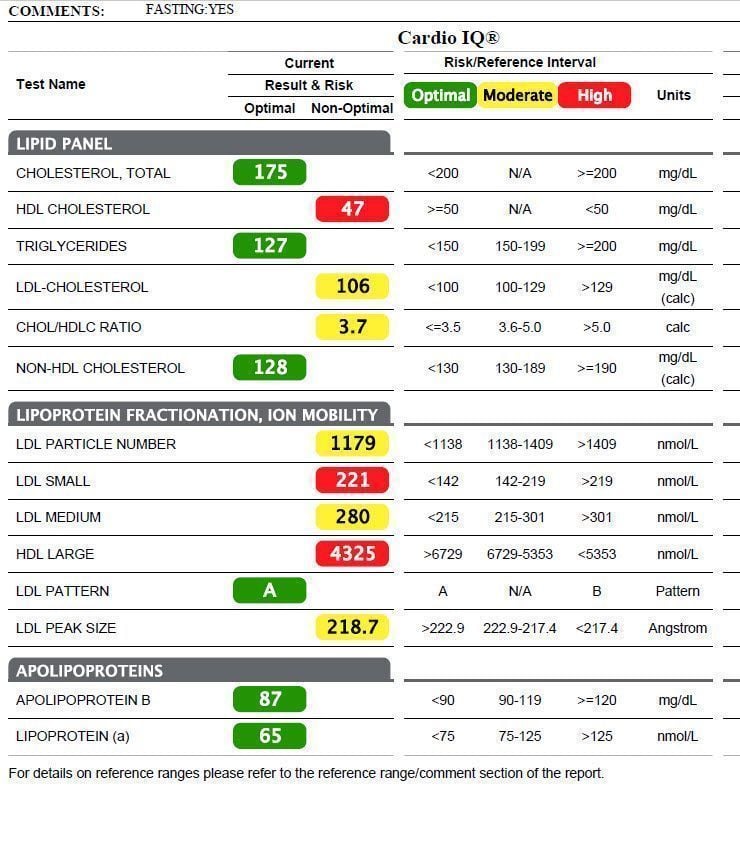
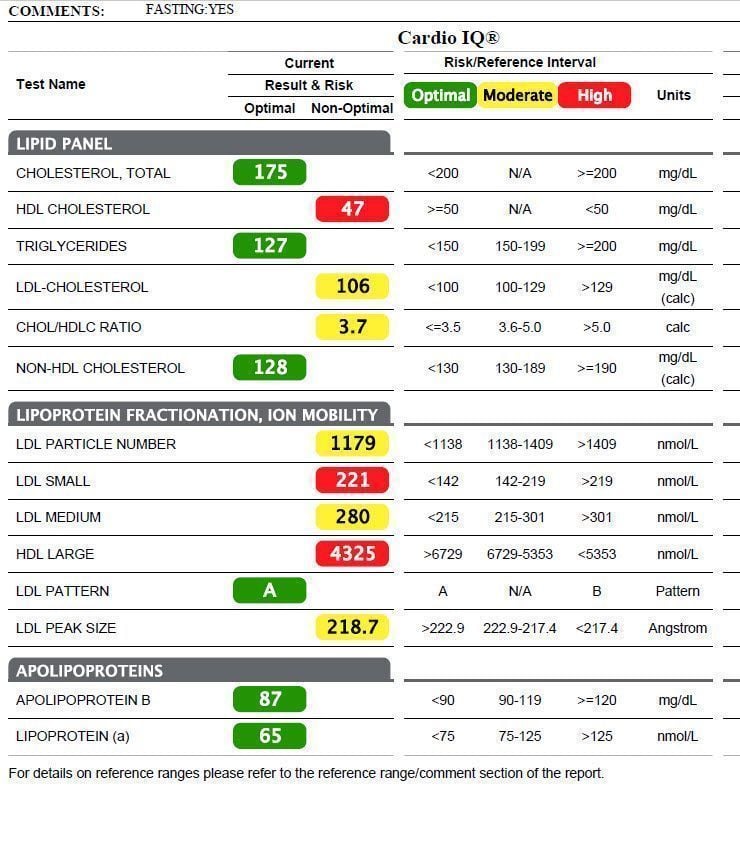
Best Heart Disease Predictor: Cardio IQ Test Guide
Discover the best heart disease predictor with Cardio IQ test. Get insights into your lipid profile and take control of your heart health.
There are a lot of articles that say vitamin K2 mk7 helps keep calcium out of arteries and puts it in the bones.
Wife and I take it. Prior to starting on the K2 my wife had a CAC score of 1500+. Haven't had it retested since. Runs in her family due to elevated Lp(a). Lipoprotein a.
Wife and I take it. Prior to starting on the K2 my wife had a CAC score of 1500+. Haven't had it retested since. Runs in her family due to elevated Lp(a). Lipoprotein a.
Nelson Vergel
Founder, ExcelMale.com
Several studies have investigated the effects of vitamin K supplementation on coronary artery calcification (CAC) scores. Here are the details of some key studies:
## AVADEC Trial
This Danish study examined the effect of high-dose vitamin K2 (720 μg/day) and vitamin D (25 μg/day) supplementation over 2 years[2][3]:
- **Participants:** 389 individuals (304 without ischemic heart disease)
- **Design:** Multicenter, double-blinded, randomized controlled trial
- **Results:**
- Overall: No significant effect on CAC progression (Δ203 vs Δ254 AU, p = 0.089)
- Subgroup with CAC scores ≥400 AU: Lower CAC progression in treatment group (Δ288 vs Δ380 AU, p = 0.047)
- Fewer safety events in treatment group (1.9% vs 6.7%, p = 0.048)
## Shea et al. Study
This study investigated the effect of phylloquinone (vitamin K1) supplementation on CAC progression[6]:
- **Participants:** 388 healthy men and postmenopausal women
- **Design:** 3-year follow-up, randomized controlled trial
- **Intervention:** 500 μg phylloquinone/day + multivitamin vs. multivitamin alone
- **Results:** No significant overall effect, but slower CAC progression in treatment group for those with baseline Agatston score >10
## Frontiers in Nutrition Systematic Review
A systematic review published in Frontiers in Nutrition analyzed multiple studies on vitamin K supplementation and vascular calcification[1]:
- Found that vitamin K supplementation has a significant effect on slowing down CAC progression
- Highlighted a study by Belling et al. showing decreased development of new calcifying lesions in the aorta and coronary arteries after 3 months of vitamin K1 supplementation
## Danish Cardiovascular Academy Study
This study examined the effect of vitamin K2 supplementation on coronary artery disease[5]:
- **Participants:** Patients with no prior coronary disease
- **Design:** 2-year follow-up, randomized controlled trial
- **Results:**
- Non-significant reduction in CAC development overall
- Significant lower progression of CAC in high-risk patients (CAC ≥400 AU)
- Reduced risk of acute myocardial infarction, revascularization, and all-cause death
While some studies show promising results, especially in high-risk individuals, the overall evidence for vitamin K supplementation in lowering calcium scores remains mixed. More research is needed to fully understand its potential benefits and identify specific populations that may benefit most from supplementation.
Citations:
[1] Frontiers | Vitamin K supplementation and vascular calcification: a systematic review and meta-analysis of randomized controlled trials
[2] Effects of vitamins K2 and D3 supplementation in patients with severe coronary artery calcification: a study protocol for a randomised controlled trial - PMC
[3] https://www.jacc.org/doi/10.1016/j.jacadv.2023.100643
[4] Vitamin K2—a neglected player in cardiovascular health: a narrative review
[5] https://academic.oup.com/eurheartj/article/43/Supplement_2/ehac544.1227/6745061?login=false
[6] Vitamin K supplementation and progression of coronary artery calcium in older men and women1 - PMC
[7] https://www.atherosclerosis-journal.com/article/S0021-9150(23)05228-0/fulltext
[8] Despite hopes, vitamin K2 supplements fail to slow calcium buildup in heart valve
## AVADEC Trial
This Danish study examined the effect of high-dose vitamin K2 (720 μg/day) and vitamin D (25 μg/day) supplementation over 2 years[2][3]:
- **Participants:** 389 individuals (304 without ischemic heart disease)
- **Design:** Multicenter, double-blinded, randomized controlled trial
- **Results:**
- Overall: No significant effect on CAC progression (Δ203 vs Δ254 AU, p = 0.089)
- Subgroup with CAC scores ≥400 AU: Lower CAC progression in treatment group (Δ288 vs Δ380 AU, p = 0.047)
- Fewer safety events in treatment group (1.9% vs 6.7%, p = 0.048)
## Shea et al. Study
This study investigated the effect of phylloquinone (vitamin K1) supplementation on CAC progression[6]:
- **Participants:** 388 healthy men and postmenopausal women
- **Design:** 3-year follow-up, randomized controlled trial
- **Intervention:** 500 μg phylloquinone/day + multivitamin vs. multivitamin alone
- **Results:** No significant overall effect, but slower CAC progression in treatment group for those with baseline Agatston score >10
## Frontiers in Nutrition Systematic Review
A systematic review published in Frontiers in Nutrition analyzed multiple studies on vitamin K supplementation and vascular calcification[1]:
- Found that vitamin K supplementation has a significant effect on slowing down CAC progression
- Highlighted a study by Belling et al. showing decreased development of new calcifying lesions in the aorta and coronary arteries after 3 months of vitamin K1 supplementation
## Danish Cardiovascular Academy Study
This study examined the effect of vitamin K2 supplementation on coronary artery disease[5]:
- **Participants:** Patients with no prior coronary disease
- **Design:** 2-year follow-up, randomized controlled trial
- **Results:**
- Non-significant reduction in CAC development overall
- Significant lower progression of CAC in high-risk patients (CAC ≥400 AU)
- Reduced risk of acute myocardial infarction, revascularization, and all-cause death
While some studies show promising results, especially in high-risk individuals, the overall evidence for vitamin K supplementation in lowering calcium scores remains mixed. More research is needed to fully understand its potential benefits and identify specific populations that may benefit most from supplementation.
Citations:
[1] Frontiers | Vitamin K supplementation and vascular calcification: a systematic review and meta-analysis of randomized controlled trials
[2] Effects of vitamins K2 and D3 supplementation in patients with severe coronary artery calcification: a study protocol for a randomised controlled trial - PMC
[3] https://www.jacc.org/doi/10.1016/j.jacadv.2023.100643
[4] Vitamin K2—a neglected player in cardiovascular health: a narrative review
[5] https://academic.oup.com/eurheartj/article/43/Supplement_2/ehac544.1227/6745061?login=false
[6] Vitamin K supplementation and progression of coronary artery calcium in older men and women1 - PMC
[7] https://www.atherosclerosis-journal.com/article/S0021-9150(23)05228-0/fulltext
[8] Despite hopes, vitamin K2 supplements fail to slow calcium buildup in heart valve
Nelson Vergel
Founder, ExcelMale.com
Based on the available research, vitamin K2 appears to be more effective than vitamin K1 in reducing coronary artery calcification (CAC) scores:
## Comparative Effects
- A cohort study of 16,057 women found that for every 10 μg increase in vitamin K2 intake, there was a 9% reduction in coronary events. In contrast, vitamin K1 intake was not significantly related to cardiovascular outcomes[2].
- The Rotterdam Study and Prospect-EPIC Study showed that high dietary intake of vitamin K2, but not vitamin K1, offered a strong positive reduction in cardiovascular risk[3].
## Vitamin K2 Specific Effects
- In the AVADEC trial, high-dose vitamin K2 (720 μg/day) supplementation over 2 years showed:
- Lower CAC progression in patients with baseline CAC scores ≥400 AU (Δ288 vs Δ380 AU, p = 0.047)
- Fewer safety events in the treatment group (1.9% vs 6.7%, p = 0.048)[6]
- Vitamin K2 helps regulate soft tissue calcification by activating matrix Gla protein (MGP), an anti-calcific protein[5].
## Vitamin K1 Effects
- While some studies show potential benefits of vitamin K1, its effects on CAC scores are less consistent:
- A study by Shea et al. found that vitamin K1 supplementation resulted in slower CAC progression for those with baseline Agatston scores >10[2].
- Bellinge et al.'s study showed that 10 mg vitamin K1 daily supplementation reduced the development of newly calcifying lesions in the coronary arteries[4].
## Mechanisms
The difference in effectiveness may be due to:
1. Vitamin K2's higher bioavailability and longer half-life compared to K1[5].
2. Vitamin K2's preferential distribution to extrahepatic tissues, where it can more effectively activate MGP[9].
While both forms of vitamin K show potential benefits, the evidence suggests that vitamin K2 may be more effective in reducing CAC scores and cardiovascular risk compared to vitamin K1. However, more research is needed to fully elucidate the comparative effects of these two forms of vitamin K on vascular calcification.
Citations:
[1] https://academic.oup.com/ckj/article/15/12/2300/6674781
[2] Vitamins K1 and K2: The Emerging Group of Vitamins Required for Human Health - PMC
[3] Highlighting The Substantial Body Of Evidence Confirming The Importance Of Vitamin K2 As A Cardio-Support Nutrient, And How The Right K2 Makes All The Difference - PMC
[4] Frontiers | Vitamin K supplementation and vascular calcification: a systematic review and meta-analysis of randomized controlled trials
[5] Vitamin K2—a neglected player in cardiovascular health: a narrative review
[6] https://bmjopen.bmj.com/content/bmjopen/13/7/e073233.reviewer-comments.pdf
[7] Association of dietary vitamin K and risk of coronary heart disease in middle-age adults: the Hordaland Health Study Cohort | BMJ Open
[8] https://ajcn.nutrition.org/article/S0002-9165(23)05148-1/fulltext
[9] https://pmc.ncbi.nlm.nih.gov/articles/PMC10351276/
[10] https://pmc.ncbi.nlm.nih.gov/articles/PMC3648716/
## Comparative Effects
- A cohort study of 16,057 women found that for every 10 μg increase in vitamin K2 intake, there was a 9% reduction in coronary events. In contrast, vitamin K1 intake was not significantly related to cardiovascular outcomes[2].
- The Rotterdam Study and Prospect-EPIC Study showed that high dietary intake of vitamin K2, but not vitamin K1, offered a strong positive reduction in cardiovascular risk[3].
## Vitamin K2 Specific Effects
- In the AVADEC trial, high-dose vitamin K2 (720 μg/day) supplementation over 2 years showed:
- Lower CAC progression in patients with baseline CAC scores ≥400 AU (Δ288 vs Δ380 AU, p = 0.047)
- Fewer safety events in the treatment group (1.9% vs 6.7%, p = 0.048)[6]
- Vitamin K2 helps regulate soft tissue calcification by activating matrix Gla protein (MGP), an anti-calcific protein[5].
## Vitamin K1 Effects
- While some studies show potential benefits of vitamin K1, its effects on CAC scores are less consistent:
- A study by Shea et al. found that vitamin K1 supplementation resulted in slower CAC progression for those with baseline Agatston scores >10[2].
- Bellinge et al.'s study showed that 10 mg vitamin K1 daily supplementation reduced the development of newly calcifying lesions in the coronary arteries[4].
## Mechanisms
The difference in effectiveness may be due to:
1. Vitamin K2's higher bioavailability and longer half-life compared to K1[5].
2. Vitamin K2's preferential distribution to extrahepatic tissues, where it can more effectively activate MGP[9].
While both forms of vitamin K show potential benefits, the evidence suggests that vitamin K2 may be more effective in reducing CAC scores and cardiovascular risk compared to vitamin K1. However, more research is needed to fully elucidate the comparative effects of these two forms of vitamin K on vascular calcification.
Citations:
[1] https://academic.oup.com/ckj/article/15/12/2300/6674781
[2] Vitamins K1 and K2: The Emerging Group of Vitamins Required for Human Health - PMC
[3] Highlighting The Substantial Body Of Evidence Confirming The Importance Of Vitamin K2 As A Cardio-Support Nutrient, And How The Right K2 Makes All The Difference - PMC
[4] Frontiers | Vitamin K supplementation and vascular calcification: a systematic review and meta-analysis of randomized controlled trials
[5] Vitamin K2—a neglected player in cardiovascular health: a narrative review
[6] https://bmjopen.bmj.com/content/bmjopen/13/7/e073233.reviewer-comments.pdf
[7] Association of dietary vitamin K and risk of coronary heart disease in middle-age adults: the Hordaland Health Study Cohort | BMJ Open
[8] https://ajcn.nutrition.org/article/S0002-9165(23)05148-1/fulltext
[9] https://pmc.ncbi.nlm.nih.gov/articles/PMC10351276/
[10] https://pmc.ncbi.nlm.nih.gov/articles/PMC3648716/
Nelson Vergel
Founder, ExcelMale.com
Vitamin K supplementation is generally considered safe for long-term use, with few reported side effects when taken at recommended doses. However, there are some potential side effects and considerations to be aware of:
## Common Side Effects
Long-term vitamin K supplementation may occasionally cause:
- Upset stomach
- Diarrhea
These side effects are usually mild and tend to resolve as the body adjusts to the supplement[3].
## Rare Side Effects
In rare cases, more serious side effects have been reported, particularly with intravenous administration:
- Allergic reactions (including anaphylaxis)
- Difficulty breathing or swallowing
- Chest tightness
- Rapid or weak pulse
- Sweating
- Dizziness or lightheadedness
- Skin rash or hives[1]
It's important to note that these severe reactions are more commonly associated with rapid intravenous administration rather than oral supplementation[1].
## Safety Considerations
1. **No Known Toxicity**: Currently, there is no known toxicity associated with high doses of vitamin K1 or K2. There is no designated upper intake level (UL) for vitamin K[2].
2. **Long-term Safety**: Vitamin K1 (10 mg daily) and vitamin K2 (45 mg daily) have been safely used for up to 2 years in studies[3].
3. **Pregnancy and Breastfeeding**: Vitamin K is likely safe when taken in recommended amounts (90 mcg daily for adults over 19 years old)[3].
4. **Interactions**: Vitamin K can interact with certain medications, particularly blood thinners like warfarin. It's crucial to consult a healthcare provider before starting supplementation if you're on any medications[3][5].
5. **Special Conditions**: People with certain health conditions, such as kidney disease, liver disease, or reduced bile secretion, may need to exercise caution or avoid high-dose supplementation[3].
## Potential Benefits of Long-term Supplementation
While not directly related to side effects, it's worth noting that long-term vitamin K supplementation may have potential benefits:
- Improved bone strength and reduced fracture risk in people with osteoporosis[3]
- Possible cardiovascular benefits, though more research is needed[7]
In conclusion, while vitamin K supplementation is generally considered safe for long-term use, it's always best to consult with a healthcare provider before starting any new supplement regimen, especially if you have pre-existing health conditions or are taking medications.
Citations:
[1] Vitamin K Side Effects: Common, Severe, Long Term
[2] Vitamin K - StatPearls - NCBI Bookshelf
[3] VITAMIN K: Overview, Uses, Side Effects, Precautions, Interactions, Dosing and Reviews
[4] Vitamin k (class) (oral route, parenteral route)
[5] Vitamin K Information | Mount Sinai - New York
[6] Vitamin K Is Essential for Bone and Heart Health—Do You Need a Supplement?
[7] https://www.tandfonline.com/doi/full/10.3402/fnr.v56i0.5329
## Common Side Effects
Long-term vitamin K supplementation may occasionally cause:
- Upset stomach
- Diarrhea
These side effects are usually mild and tend to resolve as the body adjusts to the supplement[3].
## Rare Side Effects
In rare cases, more serious side effects have been reported, particularly with intravenous administration:
- Allergic reactions (including anaphylaxis)
- Difficulty breathing or swallowing
- Chest tightness
- Rapid or weak pulse
- Sweating
- Dizziness or lightheadedness
- Skin rash or hives[1]
It's important to note that these severe reactions are more commonly associated with rapid intravenous administration rather than oral supplementation[1].
## Safety Considerations
1. **No Known Toxicity**: Currently, there is no known toxicity associated with high doses of vitamin K1 or K2. There is no designated upper intake level (UL) for vitamin K[2].
2. **Long-term Safety**: Vitamin K1 (10 mg daily) and vitamin K2 (45 mg daily) have been safely used for up to 2 years in studies[3].
3. **Pregnancy and Breastfeeding**: Vitamin K is likely safe when taken in recommended amounts (90 mcg daily for adults over 19 years old)[3].
4. **Interactions**: Vitamin K can interact with certain medications, particularly blood thinners like warfarin. It's crucial to consult a healthcare provider before starting supplementation if you're on any medications[3][5].
5. **Special Conditions**: People with certain health conditions, such as kidney disease, liver disease, or reduced bile secretion, may need to exercise caution or avoid high-dose supplementation[3].
## Potential Benefits of Long-term Supplementation
While not directly related to side effects, it's worth noting that long-term vitamin K supplementation may have potential benefits:
- Improved bone strength and reduced fracture risk in people with osteoporosis[3]
- Possible cardiovascular benefits, though more research is needed[7]
In conclusion, while vitamin K supplementation is generally considered safe for long-term use, it's always best to consult with a healthcare provider before starting any new supplement regimen, especially if you have pre-existing health conditions or are taking medications.
Citations:
[1] Vitamin K Side Effects: Common, Severe, Long Term
[2] Vitamin K - StatPearls - NCBI Bookshelf
[3] VITAMIN K: Overview, Uses, Side Effects, Precautions, Interactions, Dosing and Reviews
[4] Vitamin k (class) (oral route, parenteral route)
[5] Vitamin K Information | Mount Sinai - New York
[6] Vitamin K Is Essential for Bone and Heart Health—Do You Need a Supplement?
[7] https://www.tandfonline.com/doi/full/10.3402/fnr.v56i0.5329
Nelson Vergel
Founder, ExcelMale.com
The recommended daily dose of vitamin K for cardiovascular health is not definitively established, but research suggests that higher intakes may be beneficial. Here are the key points regarding vitamin K dosage for heart health:
## General Recommendations
The adequate intake (AI) for vitamin K, which ensures nutritional adequacy for most people, is:
- 120 micrograms (μg) per day for adult men
- 90 μg per day for adult women[5]
However, these recommendations are primarily based on vitamin K's role in blood clotting, not specifically for cardiovascular benefits.
## Dosage for Cardiovascular Health
Research indicates that higher intakes of vitamin K may be more beneficial for heart health:
- Studies have found that people with the highest vitamin K intakes had up to a 34% lower risk of atherosclerosis-related cardiovascular disease[6].
- The effective recommended dose of longer-chain menaquinones (MK-7, MK-8, and MK-9) for cardiovascular health benefits is 180–360 μg per day[1].
## Vitamin K1 vs. K2
Both forms of vitamin K have shown potential cardiovascular benefits:
- Vitamin K1 (phylloquinone): People with the highest intakes were 21% less likely to be hospitalized with cardiovascular disease related to atherosclerosis[9].
- Vitamin K2 (menaquinones): Those with the highest intakes had a 14% lower risk of hospitalization for cardiovascular disease[9].
## Safety and Upper Limit
There is no established tolerable upper intake level (UL) for vitamin K due to insufficient data on adverse effects[2]. However, this doesn't mean that extremely high doses are necessarily safe.
It's important to note that while these higher intakes show promise for cardiovascular health, more research is needed to establish definitive dosage recommendations. Additionally, individuals taking blood-thinning medications should consult their healthcare provider before increasing their vitamin K intake, as it can interact with these drugs[4].
Citations:
[1] Vitamin K2—a neglected player in cardiovascular health: a narrative review - PMC
[2] https://examine.com/supplements/vitamin-k/
[3] VITAMIN K AND HEART DISEASE – Asian Heart and Vascular Center
[4] Do You Get Enough Vitamin K?
[5] Vitamin K
[6] Growing evidence of vitamin K benefits for heart health – Nutrition & Health Innovation Research Institute
[7] Vitamin K: Health benefits, daily intake, and sources
[8] Low Levels of Vitamin K Linked to Cardiovascular Disease | dsm-firmenich Health, Nutrition & Care
[9] Diets rich in vitamin K linked to lower heart disease risk - Harvard Health
[10] New study finds growing evidence of Vitamin K value for heart health
## General Recommendations
The adequate intake (AI) for vitamin K, which ensures nutritional adequacy for most people, is:
- 120 micrograms (μg) per day for adult men
- 90 μg per day for adult women[5]
However, these recommendations are primarily based on vitamin K's role in blood clotting, not specifically for cardiovascular benefits.
## Dosage for Cardiovascular Health
Research indicates that higher intakes of vitamin K may be more beneficial for heart health:
- Studies have found that people with the highest vitamin K intakes had up to a 34% lower risk of atherosclerosis-related cardiovascular disease[6].
- The effective recommended dose of longer-chain menaquinones (MK-7, MK-8, and MK-9) for cardiovascular health benefits is 180–360 μg per day[1].
## Vitamin K1 vs. K2
Both forms of vitamin K have shown potential cardiovascular benefits:
- Vitamin K1 (phylloquinone): People with the highest intakes were 21% less likely to be hospitalized with cardiovascular disease related to atherosclerosis[9].
- Vitamin K2 (menaquinones): Those with the highest intakes had a 14% lower risk of hospitalization for cardiovascular disease[9].
## Safety and Upper Limit
There is no established tolerable upper intake level (UL) for vitamin K due to insufficient data on adverse effects[2]. However, this doesn't mean that extremely high doses are necessarily safe.
It's important to note that while these higher intakes show promise for cardiovascular health, more research is needed to establish definitive dosage recommendations. Additionally, individuals taking blood-thinning medications should consult their healthcare provider before increasing their vitamin K intake, as it can interact with these drugs[4].
Citations:
[1] Vitamin K2—a neglected player in cardiovascular health: a narrative review - PMC
[2] https://examine.com/supplements/vitamin-k/
[3] VITAMIN K AND HEART DISEASE – Asian Heart and Vascular Center
[4] Do You Get Enough Vitamin K?
[5] Vitamin K
[6] Growing evidence of vitamin K benefits for heart health – Nutrition & Health Innovation Research Institute
[7] Vitamin K: Health benefits, daily intake, and sources
[8] Low Levels of Vitamin K Linked to Cardiovascular Disease | dsm-firmenich Health, Nutrition & Care
[9] Diets rich in vitamin K linked to lower heart disease risk - Harvard Health
[10] New study finds growing evidence of Vitamin K value for heart health
Nelson Vergel
Founder, ExcelMale.com
Vitamin D3 and vitamin K2 supplementation appear to have a synergistic effect in potentially reducing coronary artery calcification (CAC), though the exact mechanisms and extent of this interaction are still being studied. Here's an overview of their interaction based on recent research:
## Synergistic Effect
The combination of vitamin K2 and vitamin D3 supplementation has shown promise in slowing down the progression of CAC, particularly in high-risk individuals[1][2]. This synergistic effect is thought to be more beneficial than supplementation with either vitamin alone.
## Mechanisms of Interaction
1. **Calcium Regulation**: Vitamin D3 enhances calcium absorption, while vitamin K2 helps direct calcium to appropriate tissues, potentially reducing inappropriate calcification in arteries[4].
2. **Protein Activation**: Vitamin K2 activates matrix Gla protein (MGP), an important inhibitor of vascular calcification. Vitamin D3 may support this process by regulating the expression of vitamin K-dependent proteins[1][4].
3. **Complementary Roles**: While vitamin D3 alone has shown limited effects on CAC progression in previous studies, its combination with vitamin K2 appears to be more effective[4].
## Research Findings
Recent studies have provided insights into the interaction of these vitamins:
- **AVADEC Trial**: This study used a combination of vitamin K2 (720 μg/day) and vitamin D3 (25 μg/day) over 2 years. While the overall results were not statistically significant, there was a trend towards reduced CAC progression in the supplemented group[1][2].
- **Subgroup Analysis**: Patients with severe CAC (scores ≥400 AU) showed a significant reduction in CAC progression when supplemented with the vitamin K2 and D3 combination[8].
- **Safety and Cardiovascular Events**: The combination supplementation was associated with fewer cardiovascular events and all-cause mortality in some studies, suggesting potential broader cardiovascular benefits[5][8].
## Limitations and Future Research
While these findings are promising, it's important to note:
1. The exact mechanisms of interaction are not fully understood and require further investigation.
2. Results have been mixed, with some studies showing significant benefits and others showing only trends or benefits in specific subgroups.
3. More research is needed to determine optimal dosages and long-term effects of combined supplementation.
Current research, including the ongoing DANCODE study, aims to further elucidate the effects of this vitamin combination on CAC and cardiovascular health[2].
In conclusion, while vitamin D3 and K2 supplementation shows promise in potentially reducing CAC progression, especially in high-risk individuals, more research is needed to fully understand their interaction and establish definitive clinical recommendations.
Citations:
[1] Effects of vitamins K2 and D3 supplementation in patients with severe coronary artery calcification: a study protocol for a randomised controlled trial - PubMed
[2] Research links vitamin K2 and D to predictor of cardiovascular disease
[3] Vitamin K2 and D May be Beneficial in Coronary Artery Calcification – Nutraceuticals World
[4] Effects of vitamins K2 and D3 supplementation in patients with severe coronary artery calcification: a study protocol for a randomised controlled trial - PMC
[5] Can You Reverse Artery Calcification With High Dose Vitamin K2? Not Really: Joel Kahn, MD: Integrative Cardiologist
[6] https://www.researchgate.net/public...dy_protocol_for_a_randomised_controlled_trial
[7] https://www.jacc.org/doi/10.1016/j.jacadv.2023.100643
[8] Effects of Vitamin K2 and D Supplementation on Coronary Artery Disease in Men: A RCT - PubMed
[9] https://www.jacc.org/doi/10.1016/j.jacadv.2023.100644
[10] https://www.kireports.org/article/S2468-0249(23)01356-6/pdf
[11] https://bmjopen.bmj.com/content/bmjopen/13/7/e073233.reviewer-comments.pdf
[12] https://academic.oup.com/eurheartj/article/43/Supplement_2/ehac544.1227/6745061?login=false
## Synergistic Effect
The combination of vitamin K2 and vitamin D3 supplementation has shown promise in slowing down the progression of CAC, particularly in high-risk individuals[1][2]. This synergistic effect is thought to be more beneficial than supplementation with either vitamin alone.
## Mechanisms of Interaction
1. **Calcium Regulation**: Vitamin D3 enhances calcium absorption, while vitamin K2 helps direct calcium to appropriate tissues, potentially reducing inappropriate calcification in arteries[4].
2. **Protein Activation**: Vitamin K2 activates matrix Gla protein (MGP), an important inhibitor of vascular calcification. Vitamin D3 may support this process by regulating the expression of vitamin K-dependent proteins[1][4].
3. **Complementary Roles**: While vitamin D3 alone has shown limited effects on CAC progression in previous studies, its combination with vitamin K2 appears to be more effective[4].
## Research Findings
Recent studies have provided insights into the interaction of these vitamins:
- **AVADEC Trial**: This study used a combination of vitamin K2 (720 μg/day) and vitamin D3 (25 μg/day) over 2 years. While the overall results were not statistically significant, there was a trend towards reduced CAC progression in the supplemented group[1][2].
- **Subgroup Analysis**: Patients with severe CAC (scores ≥400 AU) showed a significant reduction in CAC progression when supplemented with the vitamin K2 and D3 combination[8].
- **Safety and Cardiovascular Events**: The combination supplementation was associated with fewer cardiovascular events and all-cause mortality in some studies, suggesting potential broader cardiovascular benefits[5][8].
## Limitations and Future Research
While these findings are promising, it's important to note:
1. The exact mechanisms of interaction are not fully understood and require further investigation.
2. Results have been mixed, with some studies showing significant benefits and others showing only trends or benefits in specific subgroups.
3. More research is needed to determine optimal dosages and long-term effects of combined supplementation.
Current research, including the ongoing DANCODE study, aims to further elucidate the effects of this vitamin combination on CAC and cardiovascular health[2].
In conclusion, while vitamin D3 and K2 supplementation shows promise in potentially reducing CAC progression, especially in high-risk individuals, more research is needed to fully understand their interaction and establish definitive clinical recommendations.
Citations:
[1] Effects of vitamins K2 and D3 supplementation in patients with severe coronary artery calcification: a study protocol for a randomised controlled trial - PubMed
[2] Research links vitamin K2 and D to predictor of cardiovascular disease
[3] Vitamin K2 and D May be Beneficial in Coronary Artery Calcification – Nutraceuticals World
[4] Effects of vitamins K2 and D3 supplementation in patients with severe coronary artery calcification: a study protocol for a randomised controlled trial - PMC
[5] Can You Reverse Artery Calcification With High Dose Vitamin K2? Not Really: Joel Kahn, MD: Integrative Cardiologist
[6] https://www.researchgate.net/public...dy_protocol_for_a_randomised_controlled_trial
[7] https://www.jacc.org/doi/10.1016/j.jacadv.2023.100643
[8] Effects of Vitamin K2 and D Supplementation on Coronary Artery Disease in Men: A RCT - PubMed
[9] https://www.jacc.org/doi/10.1016/j.jacadv.2023.100644
[10] https://www.kireports.org/article/S2468-0249(23)01356-6/pdf
[11] https://bmjopen.bmj.com/content/bmjopen/13/7/e073233.reviewer-comments.pdf
[12] https://academic.oup.com/eurheartj/article/43/Supplement_2/ehac544.1227/6745061?login=false
Online statistics
- Members online
- 3
- Guests online
- 6
- Total visitors
- 9
Totals may include hidden visitors.
Latest posts
-
My CAC calcium score is high- Should I take vitamin K?
- Latest: Nelson Vergel
-
Low dose enclomiphene combined with Low dose TRT
- Latest: FunkOdyssey
-
-
-
© Copyright ExcelMale
















