Nelson Vergel
Founder, ExcelMale.com
What factors can falsely elevate your PSA level?
There are other factors that can affect the PSA level besides prostate cancer. The following conditions can lead to increased PSA levels:
This is the number one reason for PSA increases while on TRT.
Chronic Nonbacterial Prostatitis/Chronic Pelvic Pain Syndrome
It has been widely reported that more than 90 percent of men with prostatitis meet the criteria for chronic nonbacterial prostatitis/chronic pelvic pain syndrome (CNP/CPPS).
"Like many such poorly understood conditions, CNP/CPPS remains a challenging syndrome. Patients usually have symptoms consistent with prostatitis, such as painful ejaculation or pain in the penis, testicles or scrotum. They may complain of low back pain, rectal or perineal pain, or even pain along the inner aspects of the thighs. They often have irritative or obstructive urinary symptoms and decreased libido or impotence. As a rule, these patients do not have recurrent urinary tract infections. The physical examination is usually unremarkable, but patients may have a tender prostate."
Asymptomatic Prostatitis
Information presented at the NIH consensus conference added asymptomatic prostatitis as a new category, partly because of the widespread use of the prostate-specific antigen (PSA) test.
Clearly, symptomatic bacterial prostatitis can elevate the PSA test to abnormal levels. Asymptomatic prostatitis may also elevate the PSA level. In addition, patients who are being evaluated for other prostatic diseases may be found on biopsy to have prostatitis. There are no studies elucidating the natural history or appropriate therapy of this condition. It does appear that PSA levels return to normal four to six weeks after a 14-day course of antibiotics.23 Treatment is routinely recommended only in patients with chronic asymptomatic prostatitis known to elevate the PSA level. In these patients, it may be prudent to treat before drawing subsequent PSA samples.
Treatment of Prostatitis
From Medscape:
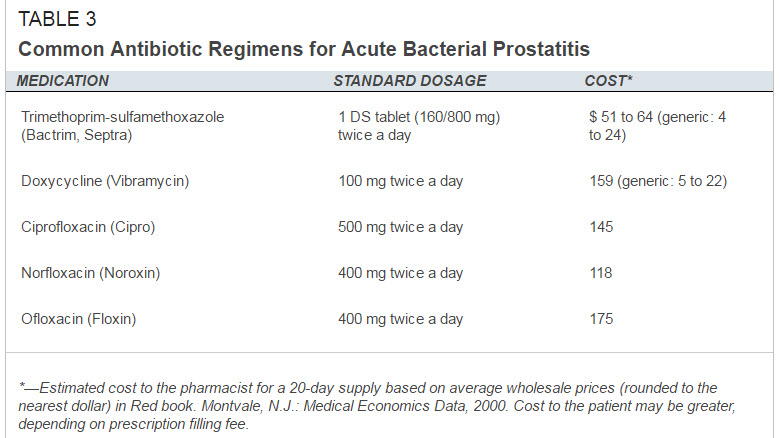
"Antibiotics that penetrate well into the acid milieu of the prostate are nonpolar and lipid-soluble and have a high measure of acid strength, a small molecular radius, and low serum protein binding. Drugs that best fit these criteria are the fluoroquinolones, doxycycline, minocycline (particularly effective against methicillin-resistant Staphylococcus aureus [MRSA]), trimethoprim (available in the United States only as trimethoprim-sulfamethoxazole [TMP-SMZ]), rifampin, and erythromycin. Of this group, the fluoroquinolones appear to achieve the best tissue levels."
 www.uspharmacist.com
www.uspharmacist.com
There are other factors that can affect the PSA level besides prostate cancer. The following conditions can lead to increased PSA levels:
- Increasing age
- Benign prostate hyperplasia (BPH), a condition that commonly develops as those assigned male at birth age and causes the prostate to grow in size
- Inflammation or infection of the prostate, like prostatitis or a urinary tract infection
- Hormone medications, like testosterone
- Ejaculation, which can raise the PSA level for a short period of time (so it’s a good idea to avoid ejaculating for a few days before the test)
- Riding a bike, or anything that puts pressure on the area near the prostate (i.e., between the genitals and the anus)
This is the number one reason for PSA increases while on TRT.
Chronic Nonbacterial Prostatitis/Chronic Pelvic Pain Syndrome
It has been widely reported that more than 90 percent of men with prostatitis meet the criteria for chronic nonbacterial prostatitis/chronic pelvic pain syndrome (CNP/CPPS).
"Like many such poorly understood conditions, CNP/CPPS remains a challenging syndrome. Patients usually have symptoms consistent with prostatitis, such as painful ejaculation or pain in the penis, testicles or scrotum. They may complain of low back pain, rectal or perineal pain, or even pain along the inner aspects of the thighs. They often have irritative or obstructive urinary symptoms and decreased libido or impotence. As a rule, these patients do not have recurrent urinary tract infections. The physical examination is usually unremarkable, but patients may have a tender prostate."
Asymptomatic Prostatitis
Information presented at the NIH consensus conference added asymptomatic prostatitis as a new category, partly because of the widespread use of the prostate-specific antigen (PSA) test.
Clearly, symptomatic bacterial prostatitis can elevate the PSA test to abnormal levels. Asymptomatic prostatitis may also elevate the PSA level. In addition, patients who are being evaluated for other prostatic diseases may be found on biopsy to have prostatitis. There are no studies elucidating the natural history or appropriate therapy of this condition. It does appear that PSA levels return to normal four to six weeks after a 14-day course of antibiotics.23 Treatment is routinely recommended only in patients with chronic asymptomatic prostatitis known to elevate the PSA level. In these patients, it may be prudent to treat before drawing subsequent PSA samples.
Treatment of Prostatitis
From Medscape:
"Antibiotics that penetrate well into the acid milieu of the prostate are nonpolar and lipid-soluble and have a high measure of acid strength, a small molecular radius, and low serum protein binding. Drugs that best fit these criteria are the fluoroquinolones, doxycycline, minocycline (particularly effective against methicillin-resistant Staphylococcus aureus [MRSA]), trimethoprim (available in the United States only as trimethoprim-sulfamethoxazole [TMP-SMZ]), rifampin, and erythromycin. Of this group, the fluoroquinolones appear to achieve the best tissue levels."
Treating Prostatitis Effectively: A Challenge for Clinicians
Last edited:

















