Nelson Vergel
Founder, ExcelMale.com
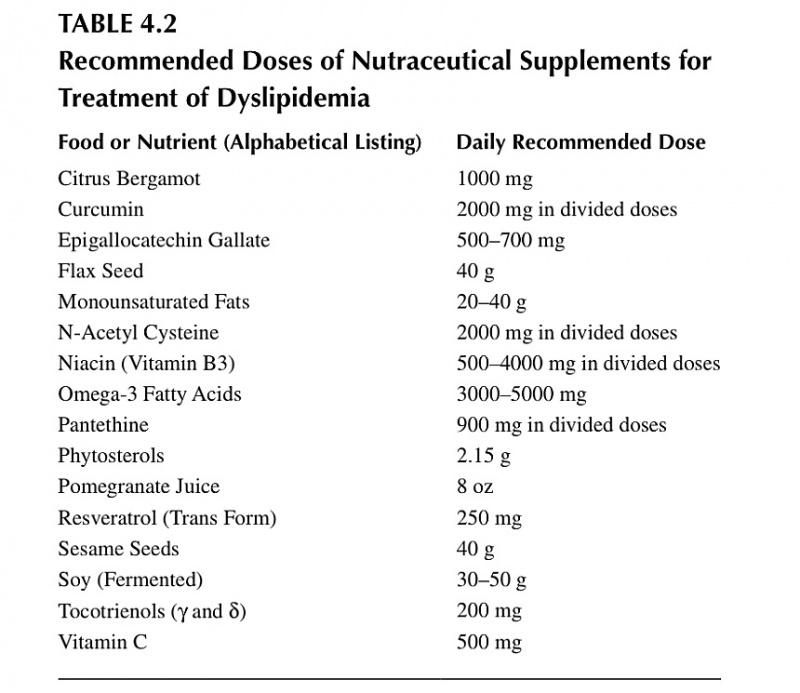
This is a very good summary table of different supplements that have been successfully studied in decreasing LDL cholesterol and triglycerides. Some also can increase HDL (good) cholesterol.
Hen measuring LDL have any of you looked at the size of LDL particles rather than just volume?
THANKS VINCE
There is a lot of very interesting information there. However, whoever that person is that said that LDL below 70 is a myth and based on the fact that babies don't have plaque cannot be taken seriously. I find it astounding that someone would make such a statement. LDL below 70 is based on RCT that have shown that lowering LDL results in less events. We never had the 70 threshold of LDL before that was proven in trials. However, we have know forever that babies have low cholesterol. The JUPITER trial has even hinted that LDL as low as 50 may reverse plaque