Nelson Vergel
Founder, ExcelMale.com
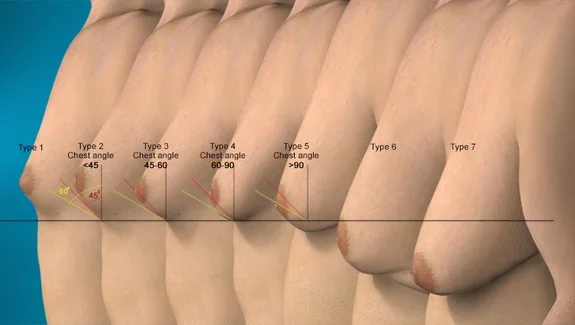
If a specific cause of gynecomastia can be identified and treated during the painful proliferative phase, there may be regression of the breast enlargement. This regression most often occurs with discontinuation of an offending drug or after initiation of testosterone treatment for primary hypogonadism. If the gynecomastia is drug-induced, decreased tenderness and softening of the glandular tissue will usually be apparent within 1 month after discontinuation of the drug. However, if the gynecomastia has been present for more than 1 year, it is unlikely to regress substantially, either spontaneously or with medical therapy, because of the presence of fibrosis. In such circumstances, surgical subcutaneous mastectomy, ultrasound-assisted liposuction, and suction-assisted lipectomy are the best options for cosmetic improvement, as described in several case series.
During the rapid, proliferative phase, manifested clinically as breast pain and tenderness, medical therapy may be attempted. Most studies of drugs -- including testosterone (in patients without hypogonadism), dihydrotestosterone, danazol, clomiphene citrate, tamoxifen, and testolactone -- have been uncontrolled and thus difficult to interpret because gynecomastia may resolve spontaneously. The few randomized, double-blind, placebo-controlled trials generally have been limited by small samples.
Although not approved for the treatment of gynecomastia, the selective estrogen-receptor modulator tamoxifen, administered orally at a dose of 20 mg daily for up to 3 months, has been shown to be effective in randomized and nonrandomized trials, resulting in partial regression of gynecomastia in approximately 80% of patients and complete regression in about 60%.36 -45 Patients in whom tamoxifen is effective usually experience a decrease in pain and tenderness within 1 month. In a retrospective analysis of a series of patients with idiopathic gynecomastia, 78% of patients treated with tamoxifen had complete resolution of gynecomastia, as compared with only 40% of patients receiving danazol. In case series describing the use of tamoxifen for this condition in more than 225 patients, adverse events were uncommon; they included epigastric distress in 2 patients and a post-traumatic deep-vein thrombosis in 1 patient.
The aromatase inhibitor anastrozole was not shown to be more effective than placebo in a randomized, double-blind, placebo-controlled trial in boys with pubertal gynecomastia. Although in an uncontrolled study of 10 patients with pubertal gynecomastia, the selective estrogen-receptor modulator raloxifene was shown to result in more than a 50% decrease in the size of the gynecomastia in the majority of the boys, there are insufficient data to recommend its use at this time.
It has also been suggested that therapy with tamoxifen may prevent the development of gynecomastia in men receiving monotherapy with high doses of bicalutamide (Casodex) for prostate cancer. In a randomized, double-blind, controlled trial involving men receiving high-dose bicalutamide (150 mg per day), gynecomastia occurred in 10% of patients who received tamoxifen at a dose of 20 mg daily, but it occurred in 51% of those who received anastrozole at a dose of 1 mg daily and in 73% of those who received placebo, over a period of 48 weeks; mastalgia occurred in 6%, 27%, and 39% of these patients, respectively. In another trial involving 3 months of therapy, gynecomastia, mastalgia, or both occurred in 69.4% of patients receiving placebo, 11.8% receiving tamoxifen (P<0.001 for the comparison with placebo), and 63.9% receiving anastrozole (not significantly different from the rate in the placebo group). Another randomized trial showed efficacy of a 10-mg dose of tamoxifen as prophylaxis against gynecomastia. Among patients treated with bicalutamide alone, gynecomastia occurred in 68.6% and mastalgia occurred in 56.8%. These rates were significantly lower among patients receiving one 12-Gy fraction of radiation therapy to the breast on the first day of treatment with bicalutamide (34% and 30%, respectively), and they were further reduced among patients receiving bicalutamide and tamoxifen (8% and 6%, respectively).49 Although it has been used in men treated for prostate cancer, tamoxifen is not approved by the Food and Drug Administration for this indication.
Source:
Braunstein, G. D., M.D. (2007). Gynecomastia. The New England Journal of Medicine, 357(12), 1229-1237.